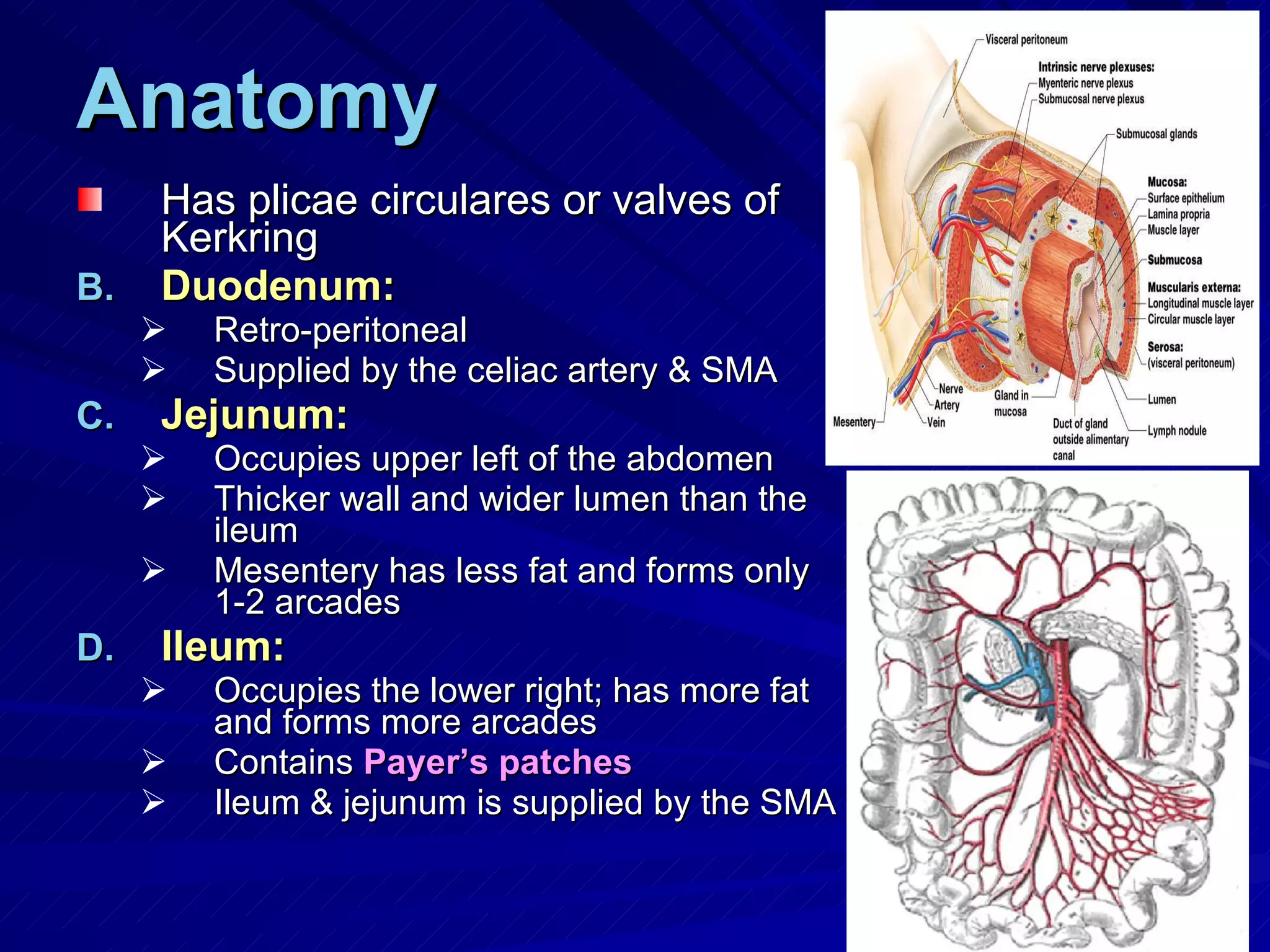
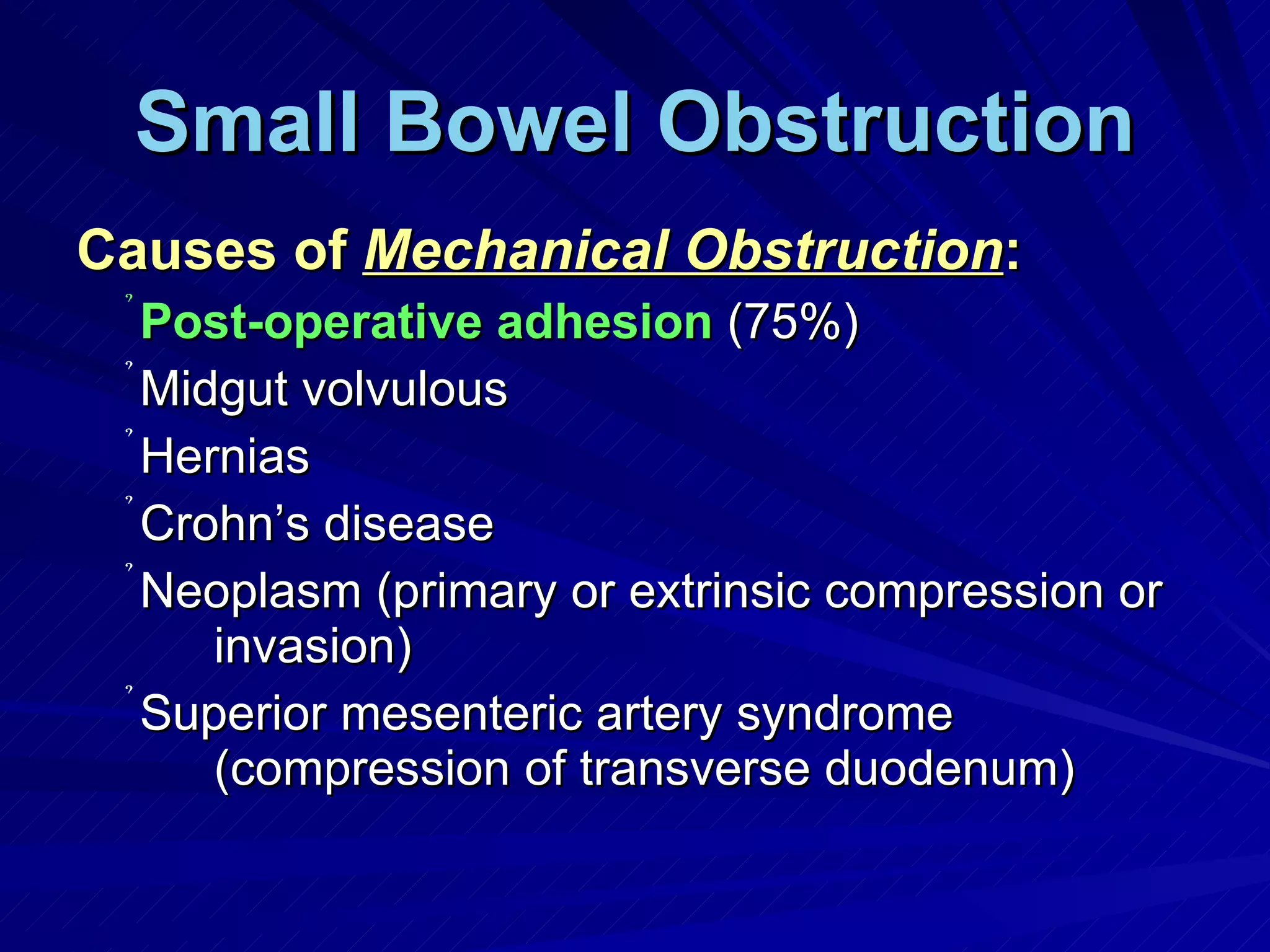
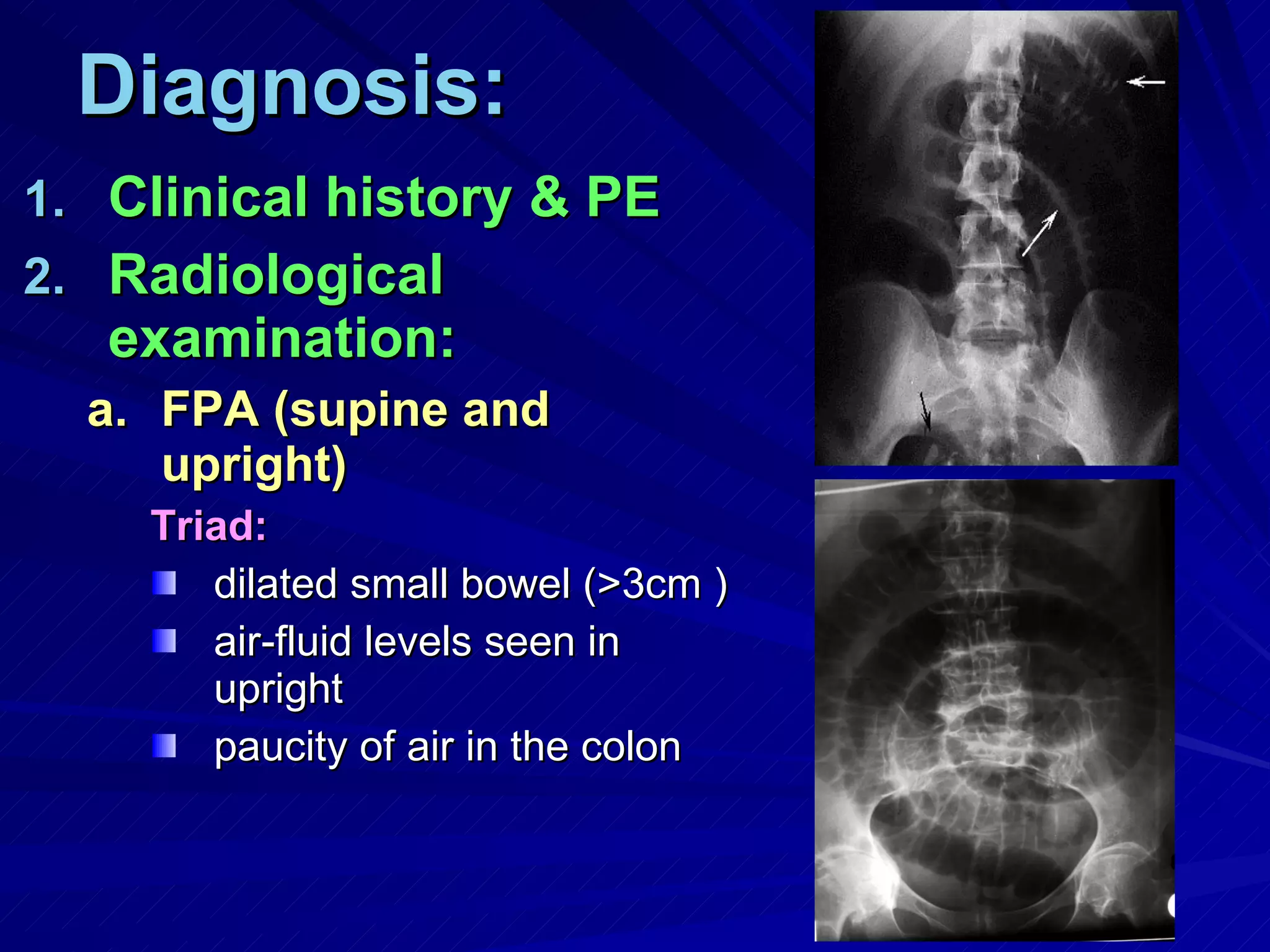
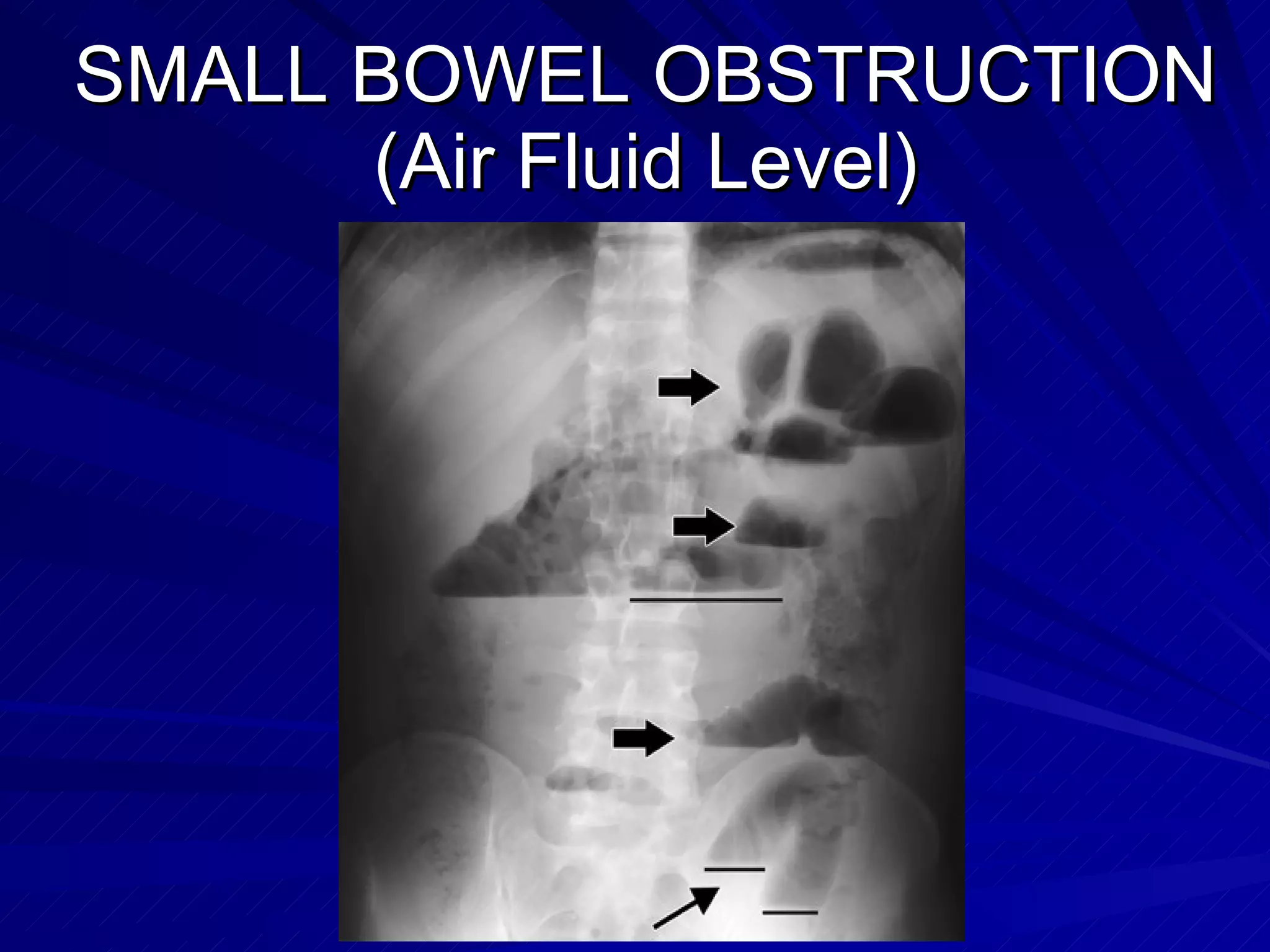
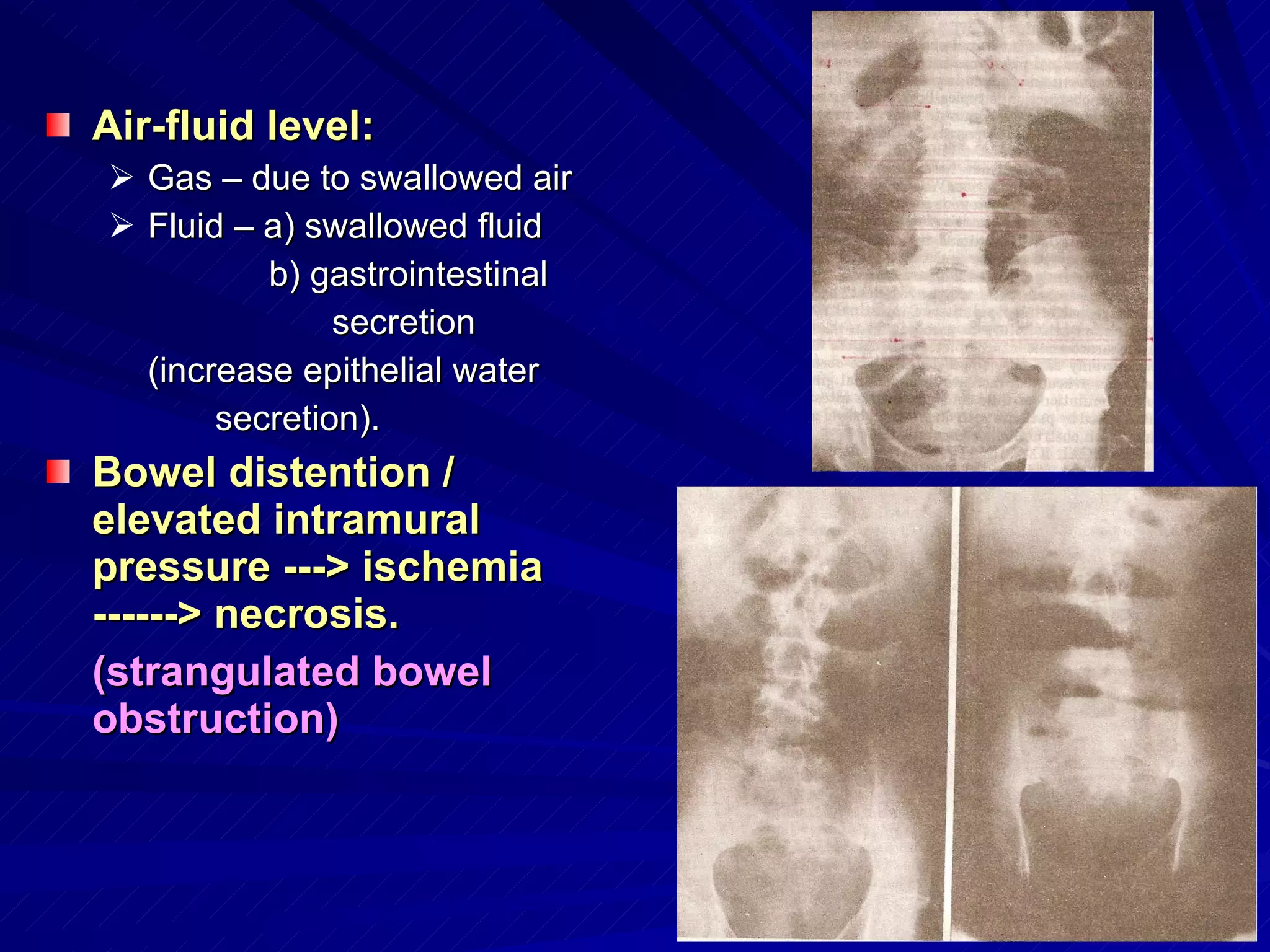
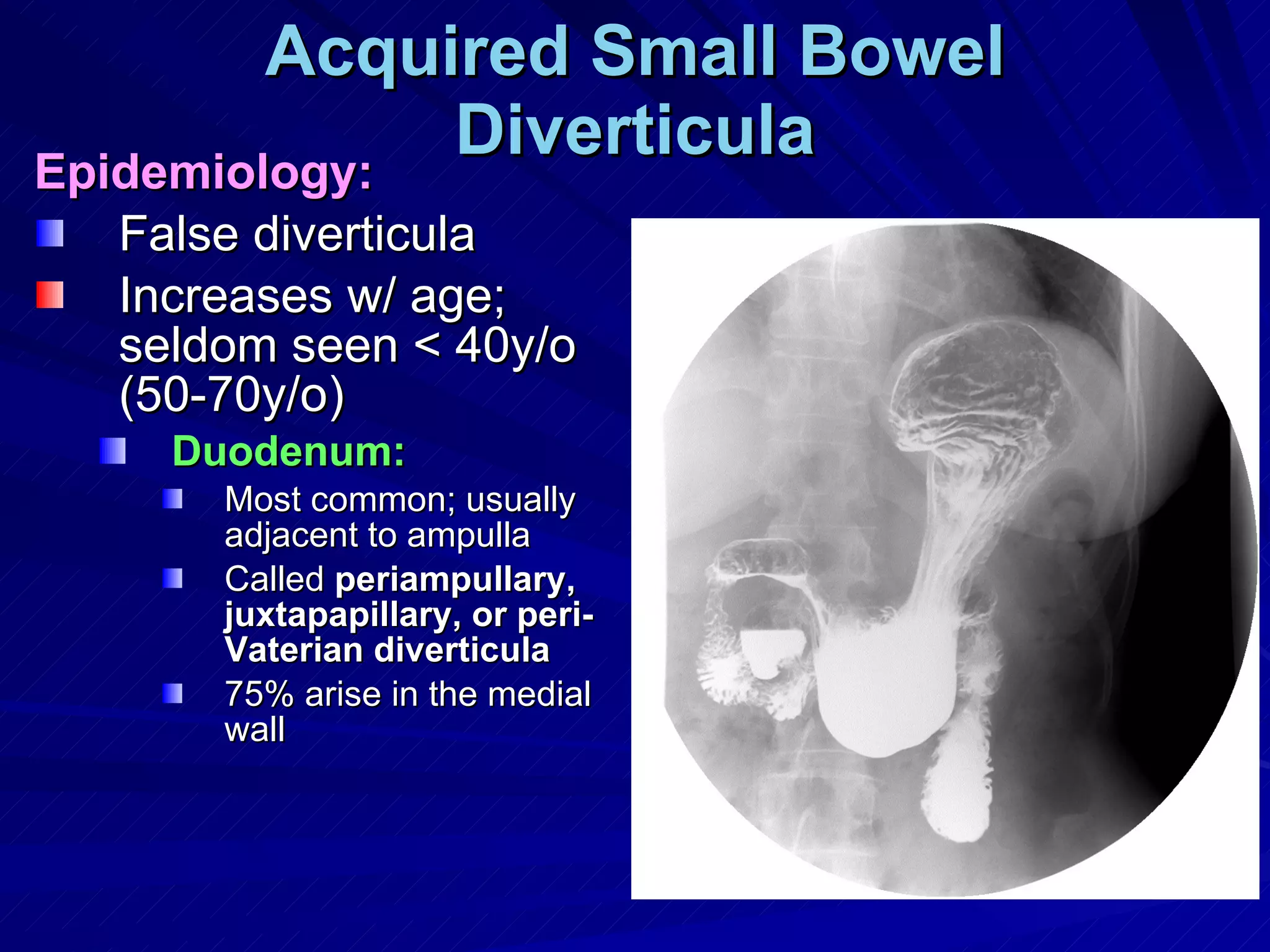
The small intestine is responsible for digestion and absorption of nutrients. It has three parts - duodenum, jejunum, and ileum. Common surgical conditions of the small intestine include small bowel obstruction, infections, inflammation, tumors, and diverticula. Mechanical obstruction from adhesions is the most common cause of small bowel obstruction. Strangulated obstruction can lead to ischemia and necrosis if not treated promptly.