Life Cycle Nutrition - Talks about the nutrition requirements for an individual in each stage of life from fetus to adulthood
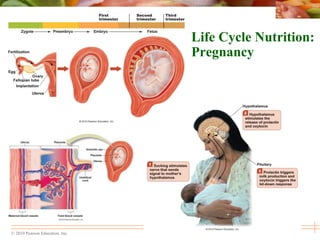
- 1. © 2010 Pearson Education, Inc. Life Cycle Nutrition: Pregnancy
- 2. © 2010 Pearson Education, Inc. Stages of Pregnancy and Importance of the Placenta During pregnancy, the diet must support the health of a woman and her growing baby Full-term pregnancy averages 38 weeks from conception to birth (divided into three trimesters)
- 3. Figure 17.1 Stages of Pregnancy and Fetal Development
- 4. © 2010 Pearson Education, Inc. Stages of Pregnancy and Importance of the Placenta Nutrients are delivered to and wastes are transported from the developing embryo through the placenta • Prevents passage of red blood cells, bacteria, and many large proteins from mother to fetus • Alcohol, drugs, and other potentially harmful substances can cross the placenta • Releases hormones required to support the physiological changes of pregnancy
- 6. © 2010 Pearson Education, Inc. Stages of Pregnancy and Importance of the Placenta Critical periods impact fetal development • Periods of rapid cellular activity are highly vulnerable to nutritional deficiencies, toxins, and other insults - Famine associated with a high cumulative incidence of heart disease - Inadequate iron during early pregnancy associated with poor cognitive development • Metabolic or fetal programming may be able to alter how genes are expressed during critical periods of development
- 7. Figure 17.3 Critical Periods of Development
- 8. © 2010 Pearson Education, Inc. Quick Review A healthy pregnancy lasts 38 weeks and is divided into three trimesters The placenta is the site through which the developing fetus accesses the mother’s organ systems for respiration, absorption, and excretory purposes Harmful toxins or inadequate nutrition can cause irreversible damage to the fetus, especially during critical periods Metabolic programming examines the interaction of the prenatal environment on genetic and other factors to produce permanent change
- 9. © 2010 Pearson Education, Inc. Nutrients and Behaviors Are Important for a Healthy Pregnancy—The Father Before conception, fathers-to-be need to eat well for healthy sperm production • Smoking, alcohol and drug abuse, and obesity are associated with decreased sperm production and function • Zinc, folate, and antioxidants are associated with healthy sperm
- 10. © 2010 Pearson Education, Inc. Nutrients and Behaviors Are Important for a Healthy Pregnancy—The Mother Before conception, mothers need to adopt a healthy lifestyle • Attain a healthy weight before conception - Obesity and overweight are associated with infertility, pregnancy complications, potential birth defects - Underweight women are at risk of delivering low birth weight or small for gestational age babies • Get plenty of folic acid–400 micrograms daily - Reduces risk of neural tube defects • Moderate fish and caffeine consumption
- 11. © 2010 Pearson Education, Inc. Nutrients and Behaviors Are Important for a Healthy Pregnancy—The Mother • Avoid cigarettes, alcohol, and illicit drugs - Smoking increases the risk of infertility, a low birth weight baby, stunted growth or intellectual development, and sudden infant death syndrome (SIDS) - Drinking alcohol during pregnancy can lead to fetal alcohol spectrum disorders (FASD); pregnant women are advised to abstain completely from alcohol
- 12. © 2010 Pearson Education, Inc. Nutrients and Behaviors Are Important for a Healthy Pregnancy • Managing chronic conditions - Diabetes, hypertension or sexually transmitted disease can increase maternal and fetal complications if not controlled before conception - Medications may be contraindicated during pregnancy, so prepregnancy counseling is essential
- 13. © 2010 Pearson Education, Inc. Quick Review Good nutrition and healthy lifestyle habits before conception are important for both men and women Factors such as smoking, alcohol abuse, and obesity decrease sperm production and function Conception is easier for women if they are at a healthy body weight Getting plenty of folic acid, avoiding fish high in methylmercury, limiting caffeine consumption, avoiding cigarettes, alcohol and drugs, and managing chronic conditions are essential for a healthy pregnancy Proper nutrition and a healthy lifestyle can prevent birth defects and may reduce future health risks
- 14. © 2010 Pearson Education, Inc. Nutrition During the First Trimester Morning sickness • Begins during the first trimester and often ends by the 20th week of pregnancy • Cause is unknown, but estrogen is thought to play a role • Small, frequent meals, avoiding an empty stomach, high carbohydrate foods, ginger, and salty foods combined with sour and tart beverages help manage nausea • Vitamin B6 may reduce nausea and vomiting • In rare cases, women experience hyperemesis gravadarum, severe vomiting which can lead to dehydration, electrolyte imbalances, weight loss and may require hospitalization
- 15. © 2010 Pearson Education, Inc. Nutrition During the First Trimester Cravings • Researchers have not found a physiological explanation for food cravings • Pica is the abnormal, compulsive intake of nonedible items such as laundry starch, burnt matches, clay, dirt, paint chips, and/or baking soda - More common in African-American women and associated with low blood levels of iron
- 16. © 2010 Pearson Education, Inc. Nutrition During the First Trimester Avoiding botanicals • Botanicals are parts of a plant believed to have medicinal or therapeutic effects • Herbs such as blue cohosh, juniper, goldenseal and raspberry tea may cause contractions of the uterus leading to miscarrage or premature labor
- 18. Figure 17.5 Components of Weight Gain During Pregnancy
- 19. © 2010 Pearson Education, Inc. Nutrition During the First Trimester Dietary considerations • 50% increase in needs for folate, zinc, and iron • Kilocalorie needs are not significantly increased during the first trimester • Focus should be on intake of nutrient-dense foods • A prenatal supplement is necessary • Vegetarians and vegans should be mindful of meeting needs for essential fatty acids and vitamin B12 • Drink milk to meet needs for calcium and vitamin D
- 20. © 2010 Pearson Education, Inc. Nutrition During the First Trimester Foodborne illness • The immune system is weakened during pregnancy, so mother and baby are at greater risk • Listeria monocytogenes may cause miscarriage, premature labor, low birth weight, developmental problems, or infant death • Pregnant women should avoid raw or undercooked meats, fish, or poultry; unpasteurized milk, cheese, and juices; and raw sprouts
- 21. © 2010 Pearson Education, Inc. Quick Review Women commonly experience morning sickness and cravings during the first trimester of pregnancy Recommended weight gain during pregnancy depends on prepregnancy weight The needs for many nutrients are increased during pregnancy, but most can be met with a balanced diet It is difficult to consume adequate iron from foods during pregnancy, so a supplement is often prescribed Pregnant women should avoid excess amounts of preformed vitamin A and D Risk of foodborne illness is increased during pregnancy, so women should handle raw foods carefully and avoid certain raw, undercooked, or unpasteurized foods
- 22. © 2010 Pearson Education, Inc. Nutrition During the Second Trimester Consume adequate kilocalories, carbohydrate, and protein • An additional 340 kcals daily is needed during the second trimester • Need a minimum of 175 grams carbohydrate per day • Protein needs increase 35% to about 71 grams daily
- 23. © 2010 Pearson Education, Inc. Activity During the Second Trimester 30 minutes or more of moderate exercise on most days is recommended Low-impact activities pose less risk for injury to mother or baby Must take care to avoid significant increases in body core temperature and drink plenty of fluids to avoid dehydration
- 25. © 2010 Pearson Education, Inc. Complications During the Second Trimester Potential complications: gestational diabetes and hypertension Gestational diabetes occurs when a woman develops high blood glucose levels during her pregnancy • May result in macrosomia, jaundice, breathing problems, birth defects, or hypoglycemia after birth • Eating healthfully, maintaining a healthy weight, and exercising regularly can reduce risk
- 26. © 2010 Pearson Education, Inc. Complications During the Second Trimester Pregnancy-induced hypertension includes three categories • Gestational hypertension – occurs early in pregnancy in women with no history of hypertension • Preeclampsia – characterized by hypertension, severe edema and protein losses in the urine; deprives fetus of oxygen and nutrient rich blood from the placenta • Eclampsia – can cause seizures and is a major cause of death of women during pregnancy The only cure for preeclampsia and eclampsia is to deliver the baby
- 27. © 2010 Pearson Education, Inc. Quick Review Pregnant women need to consume an additional 340 kcals during the second trimester Exercise can provide numerous benefits during pregnancy, but should be limited to low-impact activities to reduce risk of injury to Mom or baby Complications that often appear during the second trimester of pregnancy include gestational diabetes and pregnancy induced hypertension; women with these conditions should be closely monitored by a health care professional
- 28. © 2010 Pearson Education, Inc. Nutrition During the Third Trimester Eating frequent small meals and a high-fiber diet can help with heartburn and constipation • An extra 450 kcals are needed during the third trimester • The growing baby exerts pressure on the Mom’s intestines and stomach which can cause heartburn • Hormonal changes slow movement of food through the GI tract which may cause constipation
- 29. © 2010 Pearson Education, Inc. Special Concerns of Younger or Older Mothers-to-Be Teenage mothers • Still growing, therefore nutrient needs are even higher than an adult woman, yet more likely to have an unbalanced diet • More likely to develop pregnancy-induced hypertension, iron-deficiency anemia, and deliver premature babies Older mothers • Higher risk for complications including gestational diabetes and pregnancy-induced hypertension • Babies are more likely to have Down syndrome or other developmental disabilities
- 31. © 2010 Pearson Education, Inc. NUTRIONAL NEEDS DURING LACTATION
- 32. © 2010 Pearson Education, Inc. Breast-Feeding Lactation - A physiological process of female mammals that occurs right after pregnancy when a mother’s breast secrets milk and suckles the offspring • The “breast is best” when nourishing an infant
- 33. Figure 17.8 The Letdown Response
- 34. © 2010 Pearson Education, Inc. Composition of Breast Milk Nutrients Breastmilk contains all the nutrients the infant needs for proper growth and development Free water Proteins – Protein accounts for 75% of the nitrogen-containing compounds and the non-protein nitrogen substances include urea, nucleotides, peptides, free amino acids and DNA. Fats – Essential fatty acids and long-chain polyunsaturated fatty acids Carbohydrates – The principal carbohydrate of human milk is lactose. Minerals, vitamins, and trace elements.
- 35. © 2010 Pearson Education, Inc. Key Nutrients Found in Breastmilk Component Mean value for mature breastmilk (per 100mL) Energy (kJ) 280 Energy (kcal) 67 Protein (g) 1.3 Fat (g) 4.2 Carbohydrate (g) 7.0 Sodium (mg) 15 Calcium (mg) 35 Phosphorus (mg) 15 Iron (mcg) 76 Vitamin A (mcg) 60 Vitamin C (mg) 3.8 Vitamin D (mcg) 0.01 Source: NHMRC Dietary Guidelines for Children and Adolescents in Australia,
- 36. © 2010 Pearson Education, Inc. Composition of Breastmilk Non-nutritional components such as: • Antimicrobial factors • Digestive enzymes • Hormones and growth factors • These are important for passive protection against infections and immune-mediated diseases and modulate immunological development
- 37. © 2010 Pearson Education, Inc. Composition of Breastmilk Immune-related components and growth factors include: Secretory IgA – Predominant immunoglobulin in breast milk Bioactive cytokines – Including transforming growth factor-b (TGF-b) 1 and 2 and interleukin-10 (IL-10)] Others – leukocytes, oligosaccharides, lysozyme, lactoferrin, adiponectin, interferon-g, epidermal growth factor (EGF) and insulin-like growth factor (IGF)-1.
- 38. © 2010 Pearson Education, Inc. Composition of Breastfeeding - colostrum contains antibodies and white blood cells which protect the newborn from infections - Breast milk also contains bifidus factors, which favor the growth of the “friendly” bacterium Lactobacillus bifidus in the infant’s digestive tract, so that other, harmful bacteria cannot become established - It also protects against allergies
- 39. © 2010 Pearson Education, Inc. Benefits of Breast-Feeding Breast-feeding provides nutritional and health benefits for infants • Nutritional composition of breast milk changes as the infant grows • Colostrum is lower in fat, higher in protein, vitamin A, minerals, and antibodies • Breast milk is high in lactose, fat, B vitamins and lower in fat-soluble vitamins, sodium, and other minerals • The American Academy of Pediatrics recommends supplementing breast-fed babies with vitamin D drops to meet needs
- 40. © 2010 Pearson Education, Inc. Benefits of Breast-Feeding Breast-feeding protects against infections, allergies, and chronic disease and may enhance brain development • Provides beneficial compounds including antioxidants, hormones, enzymes, and growth factors • If continued beyond six months, may reduce risk of childhood obesity • Breast milk is rich in docosahexaenoic acid (DHA) and arachidonic acid (AA) which are important for development of vision and the central nervous system
- 41. © 2010 Pearson Education, Inc. Benefits of Breastfeeding for Mother Contracts the uterus Delays the return of regular ovulation, thus lengthening birth intervals (is not, however, a dependable method of contraception) •Conserves iron stores (by prolonging amenorrhea) May protect against breast and ovarian cancer and reduce the risk of diabetes (type 2)
- 42. © 2010 Pearson Education, Inc. Benefits of Breastfeeding Cost savings from not needing medical treatment for childhood illnesses or time off work to care forthem Cost savings from not needing to purchase formula (even after adjusting for added foods in the diet of a lactating mother) Environmental savings to society from not needing to manufacture, package, and ship formula and dispose of the packaging Convenience of not having to shop for and prepare formula
- 43. © 2010 Pearson Education, Inc. Duration of Breastfeeding Breastmilk can be provided exclusively for around the first 6 months, meeting all of the Infants nutritional needs Once complementary foods are introduced breastmilk continues to provide important nutrients and growth factors up to 2 years. The WHO recommends breastmilk continue to be part of the young child’s diet, to 2 years of age and beyond.
- 44. © 2010 Pearson Education, Inc. Maternal Energy and Nutrient During Lactation Energy Intake • A pregnant woman produces about 600ml of milk each with variation from woman to woman and in the same woman from time to time, depending primarily on the infants demand for milk • To produce adequate supply, a woman needs extra energy – about 500Kcalories above her regular needs during the first six months of lactation
- 45. © 2010 Pearson Education, Inc. Maternal Energy Needs During Lactation To meet this need: She can eat extra 330Kcalories of food each day and let the fat reserves accumulated during pregnancy provide the rest Energy Nutrients Protein and fatty acid intake remain the same during lactation as during pregnancy Nursing mothers need additional carbohydrate to replace the glucose used to make lactose in the breast milk Fibre intake also increases by 1 gram
- 46. © 2010 Pearson Education, Inc. Maternal Vitamin and Mineral Needs During Lactation Calcium - Vitamin A: 1200mcg RDA :1300mg RDA: 1200mcg Potassium -Vitamin C RDA : 5100mg RDA: 115mg Zinc RDA: 14mg Iodine 290mcg
- 47. © 2010 Pearson Education, Inc.
- 48. © 2010 Pearson Education, Inc. Nutritional Needs During Lactation Water A mother who drinks more fluids does not produce more milk but to prevent dehydration She must drink a glass of water, juice or soup at each meal or anytime the baby nurses Particular foods A nursing mother can eat whatever nutritious foods she chooses But she can eliminate foods that cause discomforts to babies
- 49. © 2010 Pearson Education, Inc. Factors Affecting Lactation Maternal Weight: Women who are obese prior to pregnancy have difficulty initiating and continuing breastfeeding and producing sufficient milk Difficulty getting infants to latch on adequately to breast and positioning them properly to feed Low milk supply due to inadequate release of prolactin Cesarean deliveries delay first suckling
- 50. © 2010 Pearson Education, Inc. Factors Affecting Lactation Maternal Age Infants breastfed by adolescents mothers may grow more slowly than infants of older mother Teens can breastfeed their infants successfully by ensuring that their nutrient needs and that of their infants are adequately supplied Maternal Eating Patterns A nutritious diet is the best choice for a breastfeeding mother and her infant
- 51. © 2010 Pearson Education, Inc. Factors Affecting Lactation Maternal Health and Infant Health Breastfeeding may be ruled out by certain medical conditions in either the infant of mother HIV Infection and AIDS Mothers with HIV infections are advised not to breast feed their infants Transmission of HIV to infants is reduced when HIV exposed mothers and their infants receive antiretroviral drugs Breastfeeding may be detrimental to infants with inborn errors of metabolism such as phenylketonuria and galactosemia
- 52. © 2010 Pearson Education, Inc. Maternal and Infant Health The compatibility of chronic and infectious diseases with breastfeeding must be considered because medications and infectious agents can be transmitted to the baby via the mother’s milk Serious infectious diseases tuberculosis and hepatitis C can be life threatening and so it may be safer if nursing is eliminated Chronic diseases incompatible with nursing include cancer being treated with chemotherapy and psychiatric conditions treated with lithium Breast surgery may affect a woman’s ability to produce milk or secrete it
- 53. © 2010 Pearson Education, Inc. Maternal Lifestyle Choices Incompatible with Lactation Alcohol Consumption: This may alter flavour of breast milk Infants metabolize alcohol inefficiently and low doses can suppress feeding and cause sleepiness Alcohol may interfere with lactation by inhibiting the hormone oxytocin
- 54. © 2010 Pearson Education, Inc. Maternal Lifestyle Choices Incompatible with Lactation Medicinal Drugs Nursing mothers must consult their physician prior to taking any drug including herbal supplements Illicit drugs Can cause irritability, tremors, hallucinations and even death in infants Smoking Cigarette smoking reduces milk production Breast milk produces by smokers contain nicotine which alters its smell and flavour Infants of smokers gain less weight
- 55. © 2010 Pearson Education, Inc. Life Cycle Nutrition: Infancy
- 56. © 2010 Pearson Education, Inc. Learning Objectives By the end of the lecture, students should be able to: Understand physiologic developments that occur during infancy Relate the physiological developments to nutrient needs of infants Explain the principles of complementary feeding Plan four star diets for infants
- 57. © 2010 Pearson Education, Inc. Physiologic Development The first two years of life is a time of rapid growth and development Many changes occur that affect feeding and nutrient intake A healthy infant’s birthweight doubles by 4 to 6 months of age and triples by one year The length of an infants is increased by 50% in the first year and doubled by 4 years
- 58. © 2010 Pearson Education, Inc. Physiological Development The stomach of an infant increases from a range of 10ml to 20ml at birth to 200ml by 1 year, enabling them to consume more food at given time and at less frequent intervals as they grow The length of gestation, the mothers prepregnancy weight and mothers weight gain during pregnancy determine an infants birth weight After birth, the growth of an infant is influenced by genetics and nourishment
- 59. © 2010 Pearson Education, Inc. Nutrient Requirements Energy Not only do infants grow rapidly, but their energy requirement is remarkably high A new born baby requires about 450 kcalories per day Carbohydrates provide energy to all the cells of the body, especially those in the brain, which depend primarily on glucose to fuel activities An infant’s brain uses relatively more glucose than the other parts of the body—about 60 percent of the day’s total energy intake Carbohydrate should provide about 30% to 60% of energy intake of infants
- 60. © 2010 Pearson Education, Inc. Energy Requirements Fat provides most of the energy in breast milk and standard infant formula Infants younger than 1 year should consume 30g of fat per day Its high energy density supports the rapid growth of early infancy Protein is very essential to the growth of infants All of the body’s cells and most of its fluids contain protein It is the basic building material of the body’s tissues Excess dietary protein can cause problems, too, especially in a small infant. Too much protein
- 61. © 2010 Pearson Education, Inc. Energy Requirements Too much protein stresses the liver and kidneys, which have to metabolize and excrete the excess nitrogen The adequacy of an infants energy intake is determined by monitoring gains in weight, length, head circumference and weight-for-length for age plotted on growth charts Energy requirements - Age Calculation 0-3 months (89×weight of infant (Kg)- 100) + 175 4-6 months (89×weight of infant (Kg)- 100) + 56 7-12 months (89×weight of infant (Kg)- 100) + 22
- 62. © 2010 Pearson Education, Inc. Energy Requirements Protein Dietary Reference Intake for infants Age Grams/Day Grams/Kg/day 0-6 months 9.1 1.52 6- 12 months 11 1.2
- 63. Nutrient Requirements Water - 0.7L/day for infants up to 6 months - 0.8L/day from 6 months to 12 months of age - Total water includes all water contained in foods, beverages and drinking water Calcium - Adequate intake is 200mg/day for 0 to 6 months infants - 260mg/day for 6 to 12 months infants Fluoride - Upper levels of 0.7mg/day for infants 0 to 6 months - - 0.9 mg/day for infants 6 to 12 months
- 64. Feeding Infants Human Milk - Breast milk excels as a source of nutrients for infants - Its unique nutrient composition and protective factors promote optimal infant health and development throughout the first year of life Frequency and Duration of Breastfeeding - Breast milk is more easily and completely digested than formula, so breastfed infants usually need to eat more frequently than formula- fed infants do - During the first few weeks, approximately 8 to 12 feedings a day, on demand
- 65. Breastfeeding Energy Nutrients -The carbohydrate in breast milk (and infant formula) is the disaccharide lactose - In addition to being easily digested, lactose enhances calcium absorption - The amount of protein in breast milk is less than in cow’s milk, but this quantity is actually beneficial because it places less stress on the infant’s immature kidneys to excrete the major end product of protein metabolism, urea - Much of the protein in breast milk is alpha-lactalbumin, which is efficiently digested and absorbed
- 66. Breastfeeding - Breast milk contains a generous proportion of the essential fatty acids linoleic acid and linolenic acid, as well as their longer-chain derivatives arachidonic acid and DHA (docosahexaenoic acid) - Arachidonic acid and DHA are found abundantly in both the retina of the eye and the brain - Research has focused on the visual and mental development of breastfed infants and infants fed standard formula without DHA and arachidonic acid added - Breastfed infants generally score higher on tests of mental development than formula-fed infants do
- 67. Breastfeeding Vitamins - With the exception of vitamin D, the vitamins in breast milk are ample to support infant growth - The vitamin D in breast milk is low, and vitamin D deficiency impairs bone mineralization - Vitamin D deficiency is most likely in infants who are not exposed to sunlight daily, have darkly pigmented skin, and receive breast milk without vitamin D supplementation Minerals - The calcium content of breast milk is ideal for infant bone growth, and the calcium is well absorbed - Breast milk contains relatively small amounts of iron,
- 68. Breastfeeding - Breast milk contains relatively small amounts of iron, but the iron has a high bioavailability - Zinc also has a high bioavailability - Breast milk is low in sodium which is beneficial for immature kidneys Immunological Protection - In addition to nutritional benefits, breast milk offers immunological protection - Not only is breast milk sterile, but it actively fights disease and protects infants from illnesses
- 69. Breastfeeding - colostrum contains antibodies and white blood cells which protect the newborn from infections - Breast milk also contains bifidus factors, which favor the growth of the “friendly” bacterium Lactobacillus bifidus in the infant’s digestive tract, so that other, harmful bacteria cannot become established - It also protects against allergies
- 70. Infant Formula Infant Formula Composition -Formula manufacturers attempt to copy the nutrient composition of breast milk as closely as possible Risks of Formula Feeding - Infant formulas contain no protective antibodies for infants - In general, vaccinations, purified water, and clean environments in developed countries help protect infants from infections - Formulas can be prepared safely by following the rules of proper food handling and by using water that is free of contamination Contaminated formulas often cause infections, leading to diarrhea, dehydration, and malabsorption
- 71. Infant Formula Special Formulas -Standard cow’s milk-based formulas are inappropriate for some infants. Special formulas have been designed to meet the dietary needs of infants with specific conditions such as prematurity or inherited diseases Infants allergic to milk protein can drink special hypoallergenic formulas or formulas based on soy protein - soy-based formulas for vegetarians and infants with galactosemia or hereditary lactase deficiency
- 72. Introducing Cow’s Milk Whole cow’s milk is not appropriate during the first year Children one to two years of age should not be given reduced- fat, low-fat, or fat-free milk routinely; they need the fat of whole milk In some infants, particularly those younger than six months of age, whole cow’s milk may cause intestinal bleeding, which can lead to iron deficiency Cow’s milk is also a poor source of iron. Consequently, it both causes iron loss and fails to replace iron
- 73. Introducing Solid Foods/ Complementary Feeding The addition of foods to an infant’s diet should be governed by three considerations: the infant’s nutrient needs the infant’s physical readiness to handle different forms of foods the need to detect and control allergic reactions.
- 74. Complementary Feeding The process of introducing liquids and foods to infants along with breast milk when that alone is no longer sufficient to meet their nutritional requirements PRINCIPLES 1. Duration of exclusive breastfeeding and age of introduction of complementary foods Practice exclusive breastfeeding from birth to 6 months of age Introduce complementary foods at 6 months of age (180 days) while continuing to breastfeed.
- 75. Principles of Complementary Feeding 2. Maintenance of breast feeding Continue frequent, on-demand breastfeeding until 2 years of age or beyond 3. Responsive Feeding An active and interactive process Parents pay attention to baby's signals for hunger and fullness a) feed infants directly and assist older children when they feed themselves, being sensitive to their hunger and satiety cues
- 76. Responsive Feeding b) feed slowly and patiently, and encourage children to eat, but do not force them c) if children refuse many foods, experiment with different food combinations, tastes, textures and methods of encouragement d) minimize distractions during meals if the child loses interest easily e) remember that feeding times are periods of learning and love - talk to children during feeding, with eye to eye contact
- 77. Principles of Complementary Feeding 4. Safe preparation and storage of complementary foods Practice good hygiene and proper food handling by: a) washing caregivers’ and children’s hands before food preparation and eating b) storing foods safely and serving foods immediately after preparation c) using clean utensils to prepare and serve food d) using clean cups and bowls when feeding children e) avoiding the use of feeding bottles, which are difficult to keep clean
- 78. Principles of Complementary Feeding 5. Amount of complementary food needed Start at six months of age with small amounts of food and increase the quantity as the child gets older, while maintaining frequent breastfeeding The energy needs from complementary foods for infants with “average” breast milk intake in developing countries are approximately: - 200 kcal per day at 6-8 months of age - 300 kcal per day at 9-11 months of age - 550 kcal per day at 12-23 months of age. (WHO/UNICEF, 1998)
- 79. Principles of Complementary Feeding 6. Food consistency Gradually increase food consistency and variety as the infant gets older, adapting to the infant’s requirements and abilities Infants can eat pureed, mashed and semi-solid foods beginning at six months “Finger foods” (snacks that can be eaten by children alone) at 8 months Family foods by 12 months Avoid foods that may cause choking (i.e., items that have a shape and/or consistency that may cause them to become lodged in the trachea, such as nuts, whole grains and nuts, raw carrots, popcorn)
- 80. Principles of Complementary Feeding 7. Meal frequency and energy density Increase the number of times that the child is fed complementary foods as he/she gets older The appropriate number of feedings depends on the energy density of the local foods and the usual amounts consumed at each feeding For the average healthy breastfed infant, meals of complementary foods should be provided: 2-3 times per day at 6-8 months of age
- 81. 7. Meal Frequency and Energy Density 3-4 times per day at 9-11 and 12-24 months of age with additional nutritious snacks (such as a piece of fruit or bread with nut paste) offered 1-2 times per day, as desired. If energy density or amount of food per meal is low, or the child is no longer breastfed, more frequent meals may be required.
- 82. Principles of Complementary Feeding 8. Nutrient content of Complementary foods Feed a variety of foods to ensure that nutrient needs are met. Meat, poultry, fish or eggs should be eaten daily, or as often as possible Vegetarian diets cannot meet nutrient needs at this age unless nutrient supplements or fortified products are used Vitamin A-rich fruits and vegetables should be eaten daily Provide diets with adequate fat content .
- 83. 8. Nutrient Content of Complementary Foods Avoid giving drinks with low nutrient value, such as tea, coffee and sugary drinks such as soda Limit the amount of juice offered so as to avoid displacing more nutrient rich foods
- 84. Principles of Complementary Feeding 9. Use of vitamin-mineral supplements or fortified products for infant and mother Use fortified complementary foods or vitamin-mineral supplements for the infant, as needed (esp for vegetarians) .
- 85. Principles of Complementary Feeding 10. Feeding during illness Increase fluid intake during illness, including more frequent breastfeeding Encourage the child to eat soft, varied, appetizing, favorite foods After illness, give food more often than usual and encourage the child to eat more
- 86. © 2010 Pearson Education, Inc. Nutrient Needs from Childhood through Adolescence
- 87. © 2010 Pearson Education, Inc. Learning Objectives By the end of the lecture the student should be able to: Enumerate the nutrient needs of children and adolescents Safety precautions to implement when introducing complementary foods Outline the causes of obesity in children and how it can be prevented and managed
- 88. © 2010 Pearson Education, Inc. Toddlers versus Preschoolers Toddlers • 1–3 years old • Growth rate is high, but slower than infancy - Age 2: Gain 3–5 pounds, 3–5 inches Preschoolers • 3–5 years old • Need same nutrients as adults, but have - Lower energy needs - Smaller appetites - Smaller stomachs
- 89. © 2010 Pearson Education, Inc. Eating Patterns and Nutrient Needs Young children need to eat frequent, small meals and nutrient-dense foods • Energy needs: 1,000–1,600 kcal per day • Appropriate portion sizes - Child-sized plates and cups - “Mini”-sized food items
- 90. © 2010 Pearson Education, Inc. Food Safety Avoid choking hazards • Offer bite-sized pieces of food • Limit availability of - Hot dogs - Nuts or seeds - Chunks of meat, cheese, or peanut butter - Whole grapes or raisins - Hard candy or gum - Popcorn - Raw vegetables
- 91. © 2010 Pearson Education, Inc. Nutrient Needs Carbohydrate • At least half of grain intake should be from whole grains • Fiber recommendations: - Ages 1–3 years = 19 grams - Ages 4–8 years = 25 grams
- 92. © 2010 Pearson Education, Inc. Nutrient Needs Protein • RDA (toddlers) = 1.1 grams per kilogram of body weight • RDA (school-age) = 0.95 grams per kilogram of body weight Fat • Ages 2–3 years old = 30–35% of kilocalories from fat • Age 4 and over = 25–35% of kilocalories from fat
- 93. © 2010 Pearson Education, Inc. Nutrient Needs: Calcium and Iron Calcium • Necessary for healthy bone development • Ages 1–3 years need 500 milligrams per day - 8 ounces of milk provides 300 milligrams Iron • Necessary during periods of rapid growth • Good sources of iron for children include lean meats, beans, and iron-fortified cereals • Cow’s milk is a poor source of iron
- 94. © 2010 Pearson Education, Inc. Iron: Deficiency versus Toxicity Deficiency (Anemia) • Most common nutrient deficiency in young children • Can lead to developmental delays • Exacerbates attention deficit hyperactivity disorder • Associated with lead poisoning Toxicity • Leading cause of death in children under age 6 • Occurs because iron can build up in tissues and organs - Ingesting 200 milligrams of iron can be fatal
- 95. © 2010 Pearson Education, Inc. Nutrient Needs Vitamin D • American Academy of Pediatrics recommends - Ages 1–8 years consume 10 micrograms (400 IU) of vitamin D per day - Sources include fortified milk, egg yolk, and some fish - Two 8-oz glasses of milk only provides half of the recommended intake - Supplements or fortified cereals may be needed
- 96. © 2010 Pearson Education, Inc. Nutrient Needs Young children need nutrient-dense beverages • Fluid recommendations are based on body weight - Drinking too much fluid may reduce fiber or iron intake • Preferred beverages include water and milk • 100% fruit juice can be provided in moderation • Soda and sugary drinks should be avoided
- 97. © 2010 Pearson Education, Inc. Food Behaviors Eating habits form early in life • Children will adapt to foods offered to them A variety of food should be offered to young children • A child may need to be exposed to a new food at least 10 times before accepting it Division of responsibility • Parents = What, when, and where food is offered • Child = Whether or not to eat, and how much “Cleaning the plate” may encourage overeating
- 98. © 2010 Pearson Education, Inc. Food Preferences Parents have strong influence over children’s food preferences • Children model after adult behaviors, both healthy and unhealthy • Including young children in food shopping, menu planning, and meal preparation can encourage variety in their food consumption
- 99. © 2010 Pearson Education, Inc. Food Preferences Picky eating and “food jags” are common in young children • Picky eating – not wanting to try new food • Food jags – tendency to eat only a small selection of food - Very common and normal, but also temporary - Can be identified through a food diary - Long-term jags increase risk of nutrient deficiency - Solutions include - Offering a variety of food items within the preferred food type - Gradually weaning the child from the food item
- 100. © 2010 Pearson Education, Inc. Vegetarianism Young children can grow and develop normally on a well- balanced vegetarian diet • Vegetarian foods such as beans, nuts, seeds, and whole grains are high in fiber - Multiple servings per day may exceed a young child’s fiber needs • Good sources of calcium, iron, and zinc need to be included in the diet • Supplementation of vitamin B12 may be necessary
- 101. © 2010 Pearson Education, Inc. School-Aged Children Ages 6–12 years Are not fully grown • Each year, gain about 7 pounds and 2.5 inches Compared to toddlers and preschoolers they • Do not eat as many times per day • Tend to be less hungry (maintain blood glucose longer) • Can eat more food at each sitting Can impact healthy development through dietary choices Continue to develop habits based on modeling adult behaviors
- 102. © 2010 Pearson Education, Inc. Quick Review Toddlers grow at a slower rate than infants, and have smaller appetites Frequent, small meals may be needed to provide adequate kilocalories, macronutrients, calcium, iron, and vitamin D Appropriate beverages include water, milk, and 100% fruit juice Small portion sizes should be encouraged, while “cleaning the plate” should be discouraged A variety of foods should be offered, and parents should serve as role models for healthy eating “Food jags” are normal and usually temporary
- 103. © 2010 Pearson Education, Inc. Child Obesity Body Mass Index (BMI) is the measurement tool used to determine weight status • For children, the categories are - Overweight = BMI ≥ 95th percentile - At risk for overweight = BMI ≥ 85th percentile
- 104. © 2010 Pearson Education, Inc. Child Obesity What is considered child obesity? • Condition of a child’s having too much body weight for his or her height. • The use of the word “obese” to describe children is controversial What causes child obesity? • Genetics: Only a small percent of cases • Environment: Excess kilocalories, inadequate exercise • Obese parents • Prenatal overnutrition
- 105. © 2010 Pearson Education, Inc. Child Obesity: Excess Kilocalories Sources include • Regular soda, candy bars, potato chips - Many of these products are sold within school buildings through vending machines or the cafeteria - Also available in most convenience stores and shopping centers - Typically replace healthy options such as milk, water, or fresh fruits and vegetables • Increased portion sizes at meals and snacks - Occurs both within and outside of the home
- 106. © 2010 Pearson Education, Inc. Child Obesity: Food Preferences High sugar and high-fat foods are often preferred by school-aged children • This could lead to an excess kilocalorie intake These preferences are formed by • Overexposure to television advertisements featuring appealing characters or famous spokespeople • Modeling of parent or sibling eating behavior
- 107. © 2010 Pearson Education, Inc. Child Obesity: Inadequate Physical Activity Low levels of exercise occur in school-aged children due to • Increased “screen time” – exposure to a television, computer, or video games • Less access to physical education in schools • Increased use of a car for transportation
- 108. © 2010 Pearson Education, Inc. Child Obesity: Prevention American Academy of Pediatrics recommendations • Parents must ensure their children receive adequate nutrients without excess kilocalories • A variety of healthy food must be offered to children • “Screen time” must be limited to two hours or less per day
- 109. © 2010 Pearson Education, Inc. Child Obesity: Treatment Weight loss is not recommended for overweight children Weight maintenance allows for healthy growth Increased physical activity is encouraged
- 111. Figure 18.3 MyPyramid for Kids A visual tool for children and parents to understand healthy eating
- 112. © 2010 Pearson Education, Inc. MyPyramid for Kids Key messages • Be physically active every day • Choose healthier foods from each group • Eat more of some food groups than others • Eat foods from every food group every day • Make the right choices for you • Take it one step at a time
- 113. © 2010 Pearson Education, Inc. The Role of Breakfast Eating breakfast may be associated with healthy body weight among children and adolescents Many schools with the National School Lunch Program also offer a school breakfast Eating breakfast may benefit • Cognitive function, including memory • Academic performance • School attendance • Psychosocial function • Mood
- 114. © 2010 Pearson Education, Inc. Adolescence Developmental period between childhood and adulthood • Ages 9–19 years • Physical changes occur, including a growth spurt - Height increases - Weight increases due to bone growth and gains in lean body mass and body fat stores • Hormonal changes occur including the onset of menstruation for females • A healthy diet is necessary at this time to ensure adequate nutrients, especially kilocalories, protein, calcium, and iron
- 115. © 2010 Pearson Education, Inc. Nutrition-Related Behaviors Desire for independence and individuality • Making own food choices • Having own transportation to access food Influence of peers, media, and nonparent role models • Exposure to unrealistic or unsafe eating practices • May lead to adoption of damaging habits
- 116. © 2010 Pearson Education, Inc. Figure 18.4 Nutrient Needs: Calcium ½ of peak bone mass accumulates in adolescence AI for calcium = 1,300 mg for ages 9–18 years • Inadequate calcium intake can lead to low peak bone mass and is a risk factor for osteoporosis
- 117. © 2010 Pearson Education, Inc. Nutrient Needs: Iron Additional iron supports muscle growth and increased blood volume • Adolescent females need iron to support menstruation RDA for iron • Females aged 14–18 years = 15 milligrams • Males aged 14–18 years = 11 milligrams Iron deficiency is common in adolescence, especially among individuals who limit intake of enriched grains, lean meats, and legumes
- 118. © 2010 Pearson Education, Inc. Disordered Eating Disordered eating patterns are more prevalent in adolescent females than males • May be linked with poor body image or low self-esteem Teens often adopt unhealthy habits such as • Skipping meals • Using food substitutes • Taking diet pills or nutritional supplements • Purging through vomiting, laxatives, or diuretics Eating family meals promotes healthy eating patterns
- 119. © 2010 Pearson Education, Inc. Putting It All Together Toddlers and preschoolers benefit from eating frequent, small meals consisting of nutrient-dense meals Exposure to a variety of healthy foods is necessary to promote good nutrition Picky eating and “food jags” are common, temporary behaviors In childhood, obesity may result from overconsumption of kilocalories, especially in the form of soda or candy Parents can serve as good role models by choosing healthy foods for themselves at family meals Adolescence is characterized by a growth spurt which increases calcium and iron needs A teenager’s eating habits may be influenced by peers or the media
- 121. Learning Objectives By the end of the lecture, students should be able to: Describe the nutritional needs of adults Describe lifestyle behaviours that promote health among adults
- 122. Nutritional Needs of Adults Adulthood is reached when both physical and emotional maturity are achieved Stages of adulthood: -Young Adulthood: late teens to mid 40’s - Middle Adulthood: 45 through mid 60’s - Older adulthood: 65 and above
- 123. Terms life expectancy: the average number of years lived by people in a given society. The life expectancy for Ghanaians is 62.4 years life span: the maximum number of years of life attainable by a member of a species
- 124. Nutritional Needs Growth and maturation are complete by early adulthood The main focus with regards to nutrition is maintaining a healthy and active life style and preventing diet-related health diseases such as: - type 2 diabetes - cardiovascular diseases
- 125. Nutrient Needs Wise food choices, made throughout adulthood, can support a person’s ability to meet: - Physical - Emotional - mental challenges - and to enjoy freedom from disease Two goals motivate adults to pay attention to their diets: -promoting health - slowing aging
- 126. Nutrient Requirements Energy Energy needs of adults are based on age, height, weight, gender and physical activity level The Harris Benedict Energy Estimation formula Males: RMR = 66.5 + (13.75 × wt) + (5 × ht) – (6.8 × age) Females: RMR = 665 + (9.6 × wt) + (1.8 ×ht)- (4.7 × age) Note: weight is in kilograms, height is in centimeters, age in years RMR – Resting metabolic rate
- 127. Nutrient Requirements Protein The protein requirement for adults is 0.8g per kilogram body weight Carbohydrates Most of their carbohydrate intake must be from whole grains Fibre recommendations are 25g for women and 38grams for men Increasing wholegrains, fruits and vegetable intake will help them meet the recommendations Fats Fat should contribute 25 to 35% of their daily energy intake Their fat intakes should largely be from the poly and mono unsaturated sources Reduce intake of trans fats
- 128. Nutrient Requirements Iron The requirement for women is higher than men until menopause Folic Acid Adult women must consume folic acid supplements Calcium Requirement for adults 19 to 50years is 1000mg/day Vitamin D Requirement for adults is 5µg/day
- 129. Healthy Habits Lifestyle behaviors that have great influence on people’s health: Sleeping regularly and adequately Eating well-balanced meals, including breakfast, regularly Engaging in physical activity regularly Not smoking Not using alcohol, or using it in moderation Maintaining a healthy body weight