Cerebrovascular Vasospasm - Etiopathogenesis and Management
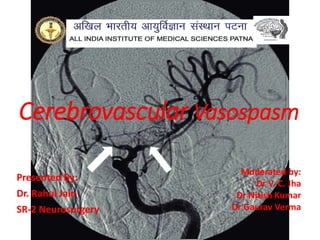
- 1. Cerebrovascular Vasospasm Presented By: Dr. Rahul Jain SR-2 Neurosurgery Moderated by: Dr V. C. Jha Dr Nitish Kumar Dr Gaurav Verma
- 2. INTRODUCTION • Cerebral vasospasm is a prolonged, sometimes severe, but ultimately reversible narrowing of the cerebral arteries that begins days after subarachnoid haemorrhage. • Bleeding significant enough to cause vasospasm is almost always due to rupture of a saccular aneurysm. • Vasospasm affects only the intradural arteries and primarily, but not exclusively, arteries and large arterioles located on the surface of the brain.
- 3. • The delayed onset and relative predictability of vasospasm provide a unique therapeutic window of opportunity not found with other types of ischemic stroke. • It remains one of the more important determinants of outcome after aneurysm rupture. • After aneurysm repair, minimizing harm from vasospasm is the mainstay of SAH management. • Vasospasm rarely complicates rupture of arteriovenous malformations, brain tumor surgery, and surgery for unruptured intracranial aneurysms because significant bleeding into the subarachnoid space is uncommon with these conditions.
- 4. Definitions 1. Radiographic vasospasm (AKA angiographic vasospasm) • Arterial narrowing demonstrated on cerebral angiography, often with slowing of contrast filling. • diagnosis is solidified by previous or subsequent angiograms showing the same vessels with normal caliber. • Peaks in severity at 1 week • Incidence - around 50% (range: 20–100%). 2. Clinical vasospasm • delayed ischemic neurologic deficit (DIND), or symptomatic vasospasm. • Clinically characterized by confusion or decreased level of consciousness sometimes with focal neurologic deficit (speech or motor).
- 5. 3. Delayed cerebral ischemia (DCI) • Presence of focal neurological deficit or a decrease of at least 2 points on the Glasgow Coma Scale score lasting longer than 1 hour with no other identifiable cause. • umbrella term that encompasses symptomatic vasospasm, delayed ischemic neurological deficit (DIND), and asymptomatic delayed cerebral infarction. 4. Early brain injury (EBI) • refers to a number of factors including the transient increase in ICP, reduction of CBF, apoptosis, and edema formation. 5. Delayed cerebral infarction • Radiologic evidence of an infarct present after the time of DCI within 6 weeks of SAH and 24 to 48 hours after aneurysm repair.
- 6. EPIDEMIOLOGY • Angiographic vasospasm typically occurs 4 to 14 days after SAH, peaking at days 7 to 10 and resolving by day 21. • Only about 40% of patients with vasospasm will develop DCI. • Rough estimates are that at least moderate vasospasm in at least one cerebral artery will develop in two-thirds of patients with ruptured aneurysms, half of these patients will become symptomatic as a result of ischemia, and delayed cerebral infarction will develop in about half of these patients.
- 7. PREDICTION • Large volume of persistent subarachnoid clot is the most important risk factor. • Modified Fisher scale
- 8. • Intraoperative aneurysm rupture during surgical clipping - not found to correlate with increased risk. • Other possible relationships -female sex, younger age, Japanese ethnicity, cocaine use, and aneurysm location with DACA aneurysms having unusually high incidence. • Endovascular coiling, as opposed to microsurgical repair of ruptured aneurysms, is associated with a lower risk. • Spontaneous perimesencephalic or prepontine SAH (or both) unassociated with aneurysm rupture is typically a low-volume haemorrhage with low risk.
- 9. PATHOGENESIS • Breakdown of subarachnoid blood clots forms haemoglobin and other by-products, such as methemoglobin, oxyhemoglobin, heme, and hemin. • These products may trigger vasospasm through vasoirritation resulting in 1. smooth muscle contraction, 2. alteration in endothelial cell function resulting in production of potent vasoconstrictors, and 3. neuroinflammation.
- 10. Smooth Muscle Contraction • Vasospasm is prolonged cerebral arterial constriction caused by vascular smooth muscle contraction. • Hemoglobin in the subarachnoid entry and release of calcium activation of calcium/calmodulin-dependent MLCK phosphorylation of myosin light chains actin- myosin cross linkage contraction • Chronic vasospasm – occurs after several days and lasts several weeks Protein kinase C, Rho kinase, and protein tyrosine kinase shortening in the absence of high intracellular calcium levels
- 11. • Contiguous and second-phase chronic vasospasm is less reversible with pharmacologic vasodilators • Sustained vasoconstriction is associated not only with functional impairment of the vessel but also with ultrastructural damage to the vascular wall layers including vacuolization of endothelial cells, loss of tight junctions, breakage of the internal elastic lamina, and patchy myonecrosis in the tunica media.
- 12. Endothelial Injury, Nitric Oxide, and Endothelin-1 • Auto-oxidation of oxyhemoglobin methemoglobin and superoxide anion radicals lipid peroxidation lipid peroxides and hydroxyl radicals permeate vessel wall endothelial injury. • Endothelial damage loss of endothelial NO synthesis (powerful vasodilator) or overproduction of endothelin-1 (ET-1 – powerful vasoconstrictor). • Oxyhemoglobin has been shown to trigger the release of ET-1 from endothelial cells, acts on neighboring vascular smooth muscle ETA receptors, and causes profound and sustained vasoconstriction.
- 13. • Decreased availability of the simple molecule NO may contribute to the development of vasospasm in the following ways: (1) Endothelial nitric oxide synthase (NOS) dysfunction in vasospastic vessels, (2) NO scavenging by oxyhemoglobin; (3) reversal of vasospasm by NO donors, (4) disappearance of neuronal NOS activity from the adventitia of vasospastic vessels, (5) decreased cerebrospinal fluid (CSF) nitrite levels along with increased levels of asymmetrical dimethyl-l-arginine, the endogenous inhibitor of NOS
- 14. Inflammation, Vessel Remodeling, and Vasospasm • Inflammatory cascades are activated after SAH, which may contribute to vasocontraction or modify the vessel wall extracellular matrix and smooth muscle cell phenotype— a process known as vascular remodelling. • Elevated serum tumor necrosis factor α, serum P- selectin, serum L-selectin, peripheral blood mononuclear cell Toll-like receptor 4 expression level, blood neutrophil count, elevated CSF interleukin-6, plasma complement C3a. • CSF neutrophil percentage of greater than 62% to be predictive of vasospasm
- 15. CLINICAL FEATURES • Symptoms of ischemia appear 1 week after aneurysm rupture, remain vigilant for this complication for at least 2 weeks after SAH. • Regular and careful bedside examination remains the simplest and most effective means of detecting early ischemia in awake patients. • Subtle findings such as diminished attention, changes in verbal output, or a slight but new pronator drift. • Symptomatic vasospasm usually gradual onset, sometimes heralded by increased headache and a change in patient behavior—either agitation or somnolence.
- 16. • Signs of symptomatic vasospasm are referable to the territory that has become ischemic. • MCA territory – monoparesis or hemiparesis and, when the dominant hemisphere is affected, aphasia. • ACA territory – leg weakness, but often bilateral confusion, drowsiness, poverty of speech, and eventually abulia are characteristic signs. • Symptomatic vasospasm is difficult to detect in patients who remain in poor neurological condition • These patients require clinical examination and additional tests like CT angio or perfusion.
- 17. • Delayed neurological deterioration after aneurysmal SAH has a number of causes apart from vasospasm. • One or more of these conditions can magnify even a focal neurological deficit and therefore easily be mistaken for vasospasm, which has a tendency to be overdiagnosed in the setting of SAH.
- 18. Diagnosis
- 19. • Diagnosis of symptomatic vasospasm requires that the other causes of delayed worsening listed earlier be ruled out. • Transcranial Doppler principle that as an artery narrows, blood flow velocity within it increases. Non invasive, bedside, easily done at bedside and can be done on daily basis provided that the patient has an adequate acoustic window in the temporal region through which to insonate. • TCD velocity of MCA and Lindegaard Ratio (VMCA/VICA)
- 20. • CTA: specific for vasospasm, but may overestimate the degree of stenosis. DSA is gold standard. • MRA: may be useful for management of vasospasm (not a practical alternative to conventional angiography as not possible in critically ill) • continuous quantitatively analyzed EEG monitoring in the ICU • decline of the percent of alpha activity (defined here as 6–14 Hz) called “relative alpha” (RA) from a mean of 0.45 to 0.17 can predict the onset of vasospasm earlier than TCD or angiographic changes • a decline of total EEG power (amplitude) was 91% sensitive for predicting vasospasm. • significant amount of manpower required for around- the-clock real-time telemetry limits its clinical use.
- 21. • Cerebral microdialysis catheters bedside measurement of extracellular concentrations of glutamate, lactate, pyruvate, lactate/pyruvate ratio, glucose, and glycerol in brain tissue. • The markers with the most reliable prediction of ischemia, are glutamate and lactate, as these peaked 24 hours before clinical ischemia. • alterations in cerebral blood flow (CBF): ○ MRI: DWI and PWI may detect early ischemia ○ CT perfusion study ○ xenon CT: may detect large global changes in CBF, but too insensitive to detect focal blood flow changes, and does not correlate with increased TCD velocities, positron emission tomography (PET), or SPECT scans (nonquantitative, and takes longer than xenon studies).
- 22. • CT perfusion is one of the most widely used investigation in patients with SAH. Perfusion hemodynamics of a selected region are seen during contrast bolus and Cerebral ischemia can be identified with side to side differences in perfusion or absolute threshold values for CBF, cerebral blood volume and mean transit time. • CTP can provide early detection of reduced CBF, prolongation of MTP which is also indicative of ischemia, and status of CBV which is normally preserved in penumbra but markedly reduced in infarcts. • Sensitivity and specificity are 74 to 97% and 76 to 93% respectively. • Major limitations are that it is non continuous and has high degree of variability owing to differences in equipment used and post-processing method.
- 23. Patient presenting with weakness of the right arm and leg, 6 days after SAH related to a ruptured saccular aneurysm of the left MCA bifurcation, which was clipped (bold arrow). DSA showed moderate vasospasm on the distal carotid segment and severe vasospasm on the A1 t of the left ACA and the M1 and proximal M2 of the left MCA (A, black arrowheads). MIP image before (B) and after (C) intra-arterial infusion of nimodipine showing resolution of the vasospasm (white arrowheads), and followed by the resolution of the symptoms. At pretreatment PCT, MTT was increased in the left MCA territory (D), CBF was normal (E), and a slight increase in CBV (F) was observed, representing vasospasm related auto regulation mechanisms.
- 24. PREVENTION OF VASOSPASM AND CEREBRAL PROTECTION • Hypovolemia in the acute stage of SAH owing to volume contraction from natriuresis and inappropriate antidiuretic hormone elevation. • systematic review on triple H therapy found no difference in clinical outcome.
- 25. • Medical morbidities associated with triple-H therapy include pulmonary edema, myocardial ischemia, hyponatremia, renal medullary washout, indwelling catheter–related complications, cerebral hemorrhage, and cerebral edema. • After aneurysm repair, circulating blood volume and systemic blood pressure should be maintained in the normal range. • Hyponatremia may increase the risk for vasospasm and is associated with cerebral infarction in poor- grade patients. Current AHA guidelines recommend salt replacement in the form of NS or 3% hypertonic saline combined with fludrocortisone (Florinef) (0.3 mg/d) administration if the patient is experiencing vasospasm.
- 26. • Blood transfusion has been associated with a higher likelihood of both vasospasm and poor outcome. • Current guidelines suggest a transfusion threshold of 8 g/dL in patients with SAH without symptomatic spasm. • Optimal ventilation and oxygenation, fever prevention,glucose control, good nutrition, and attention to concentration of all electrolytes in addition to sodium are important in reducing the impact of vasospasm and delayed ischemia.
- 27. REVERSAL OF VASOSPASM AND CEREBRAL ISCHEMIA • Augmentation of CBF through collaterals around vasospastic vessels by elevating systemic blood volume and pressure can reverse cerebral ischemia. Triple-H Therapy: Hypervolemia, Hypertension, and Hemodilution • intended to improve cardiac output, increase CPP, and optimize hemorheology for oxygen transport, and for many years was the mainstay of treatment for symptomatic vasospasm. • Significant risks and morbidities of this therapy.
- 28. • Risks are greatest in elderly patients and patients with intrinsic, preexisting cardiopulmonary disease. • deliberate triple-H therapy combining all three components has fallen out of favor in SAH management. • Current American Heart Association guidelines recommend induction of hypertension (class 1, level of evidence B) and maintenance of euvolemia (class 1, level of evidence B) for treatment of DCI. • When symptomatic vasospasm is diagnosed or strongly suspected, hemodynamic treatment should begin with volume expansion with an isotonic crystalloid infusion only if required.
- 29. • In a healthy patient, modest volume expansion can raise CBF in vasospastic territories without a significant change in cardiac indices. • A replete intravascular volume beyond which additional expansion is probably of no further benefit corresponds to a CVP between 8 mm Hg and 10 mm Hg or a PCWP between 14 mm Hg and 16 mm Hg. • Current guidelines do not recommend intentional hemodilution. • Hemodilution accompanies any deliberate volume expansion, and reduced viscosity may contribute to an improvement in oxygen delivery provided Hct doesn’t fall below 30% and Hb below 9 g/dl.
- 30. • Induced hypertension is effective in improving cerebral oxygenation in patients with vasospasm and has fewer complications than hypervolemia. • Provided that the ruptured aneurysm has been repaired, it is recommended to treat symptomatic vasospasm with the administration of a vasopressor, the most commonly used being phenylephrine or norepinephrine (α-agonist vasopressors). • Dobutamine or dopamine and another cardiac inotrope, milrinone, has also been used after SAH. • The key aspect of treatment if it is to be successful in reversing ischemia is prompt elevation of blood pressure, regardless of the agent chosen.
- 31. • 70% of patients with DCI clinically improve with induced hypertension. • If there is no clinical response to an initial target of 160 to 180 mm Hg systolic blood pressure, the target is escalated every 30 minutes to a maximal target of 220 mm Hg for SBP, 120 mm Hg for CPP, and 140 mm Hg for MAP. • If ischemic signs persist, hypertensive treatment should be considered to have failed. • The only randomized controlled trial of induced hypertension in SAH was discontinued prematurely owing to lack of benefit and slow enrollment.
- 32. Other Reversal Therapies • Some evidence for targeting a cardiac index of >4.0 L/min/m2 for the treatment of DCI. • Neurocritical Care Society guidelines suggest a transfusion target of 9 to 10 g/dL in patients with DCI, which is above the transfusion target of 8 g/dL for prevention of DCI (evidence is lacking). • Hypertonic Saline can be considered in patients who are also experiencing high ICP. • Therapeutic Hypothermia for a temperature target between 33°C and 36°C but no objective evidence
- 33. • Intrathecal/Intraventricular Vasodilators • In patients with severe and medically refractory vasospasm • Sodium nitroprusside, an NO donor, has been administered into the lateral ventricles via a ventriculostomy catheter or into the thecal sac via a lumbar drain. • Intrathecal nicardipine was found to reduce TCD velocities within 8 hours of administration. • Intra-aortic Balloon Counterpulsation and Aortic Flow Diversion • originally designed for the management of cardiogenic shock.
- 34. • transfemoral aortic balloon that inflates on aortic valve closure with each cardiac cycle and augments diastolic flow proximally to the coronary and cranial arteries and distally to the peripheral circulation. • reported to be feasible and effective in patients with combined severe vasospasm and cardiac failure. • For patients at high risk of vasospasm but normal cardiac function did not confer any clinical benefit in a small, single-center randomized controlled trial.
- 35. Endovascular Reversal of Vasospasm • Indications- When maximal medical therapy fails in patients with clinically symptomatic vasospasm. • Options include percutaneous transluminal balloon angioplasty (PTA) or transcatheter intra-arterial vasodilator infusion or their combination. • PTA is judiciously reserved for cases of severe, refractory, proximal vessel vasospasm.
- 36. • Patient previously underwent surgical clipping of a blister aneurysm of the ophthalmic segment (D, arrowhead). • Anteroposterior (A and C) and lateral (B and D) angiograms obtained before (A and B) and after (C and D) • angioplasty for severe symptomatic vasospasm. Arrows show the dramatic increase in diameter of the middle cerebral artery and distal ICA (C).
- 37. • Verapamil at 5 to 20 mg per vascular distribution (typically 5–10 mg) as first-line therapy for angiographically significant vasospasm, especially for distal spasm beyond the first-order branches of the circle of Willis. • Intra-arterial administration of verapamil has been demonstrated to be safe in dosages between 2 and 20 mg per vessel. Neurological improvement is seen in 30% to 66% of patients, and repeat treatment is necessary in only 15% of patients. • Nicardipine has a similar profile to verapamil in relative tissue selectivity, with minimal cardiac impact.
- 38. • Milrinone - better clinical results, excellent safety profile, a synergistic effect of high-dose milrinone and nimodipine infusion for endovascular rescue therapy has been reported. • To date, no evidence exists to confirm which intra- arterial agent is more efficacious for the treatment of refractory vasospasm. • Continuous intraarterial infusion of calcium channel blockers may provide additional advantages such as needing fewer transports of unstable patients into the radiology suite, allowing longer exposure to intra-arterial drug therapy, and requiring fewer arterial catheterizations, which then lessens the risk of access complications. • Drawbacks include systemic hypotension, infection, and increased ICP.
- 39. • Prophylactic PTA in patients at high risk for developing life-threatening cerebral vasospasm has been reported but remains very controversial. • In canine models of posthemorrhagic vasospasm, prophylactic PTA on day 0 prevented the development of vasospasm on day 7 in all animals. • In one small clinical series, patients with aneurysmal Fisher grade 3 SAH treated with prophylactic PTA within 3 days of hemorrhage; none of these patients developed delayed ischemic neurological deficit (DIND) or clinically significant abnormalities on transcranial Doppler imaging, but the rate of mortality secondary to vessel rupture was 8%. • Currently no guideline for prophylactic PTA.
- 40. SUGGESTED APPROACH TO PREVENTION AND TREATMENT • Patients should be kept well hydrated and euvolemic with isotonic crystalloid and intermittent albumin infusions (at least 3 L/d, combined) • ICP kept normal with external ventricular drainage, and CPP optimized to levels higher than 70 mm Hg. • No attempt should be made to lower mild or moderate hypertension. • TCD values greater than 200 cm/s in the MCA are indicative of significant angiographic vasospasm in that artery. • Regular clinical assessments searching for changes in mentation, verbal output, and arm and hand control are important; the best testing for developing vasospasm and cerebral ischemia is regular bedside neurological examinations through the vasospastic interval days 4 to 14 after SAH.
- 41. • All patients should receive nimodipine, 60 mg every 4 hours orally or via a nasogastric tube for 21 days or as long as they remain in the hospital. • Every effort should be made to avoid hyponatremia, fever, and hypoxia, and patients should be fed enterally as soon as possible. • Symptomatic vasospasm detected in patients in whom examination can be conducted and moderate to severe angiographic vasospasm in comatose, unexaminable patients should be treated by infusion of a vasopressor to induce HTN. • CVCs are preferred over peripheral IV caths.
- 42. • If signs do not respond quickly and completely or a target blood pressure is difficult to reach, endovascular treatment is indicated including angioplasty for all narrowed arteries reachable with a balloon-tipped catheter. • CT scan must be performed first to rule out a large, established infarction or a new haemorrhage. • Failure of neurological deficits to improve with hypertension and/or endovascular treatment often indicates that deterioration was due to another cause or ischemia has progressed to an established infarction.
- 45. Conclusion Treatment paradigms will continue to evolve as new medications become available, diagnostic modalities are discovered, and the pathophysiologic characteristics of vasospasm are better understood. Because of these promising future developments, vascular neurosurgeons and interventionalists should remain attuned to such changes and tailor treatment regimens accordingly.
- 46. References 1. Greenberg 10th ed 2. Youman and winn 8th ed