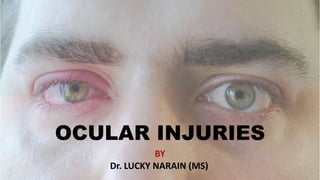
OCULAR INJURIES
- 1. OCULAR INJURIES BY Dr. LUCKY NARAIN (MS)
- 2. Damage or trauma in fl icted to the eye by external means. The concept includes both surface injuries and intraocular injuries. During trauma so ft ti ssues and bony structures around the eye maybe involved. OCULAR TRAUMA OPEN GLOBE INJURY Open-globe injury is associated with a full-thickness wound of the sclera or cornea or both. It includes rupture and lacera ti on of eyewall. CLOSED GLOBE INJURY Closed-globe injury is the one in which eyewall (sclera and cornea) does not have a full thickness wound but there is intraocular damage. It includes contusion and lamellar lacera ti on.
- 3. CLOSED GLOBE INJURY 1. Contusion refers to the closed-globe injury resul ti ng from blunt trauma. Damage may occur at the site of impact or at a distant site. 2. Lamellar lacera ti on is a closed-globe injury characterized by a par ti al thickness wound of the eyewall caused by a sharp object or blunt trauma OPENED GLOBE INJURY 1. Rupture refers to a full-thickness wound of eyewall caused by the impact of blunt trauma. 2. Laceration refers to a full-thickness wound of eyewall caused by a sharp object. a) Penetra ti ng injury refers to a single lacera ti on of eyewall caused by a sharp object which traverses the coats only once. b) Perfora ti ng injury refers to two full thickness lacera ti ons (one entry and one exit) of the eyewall caused by a sharp object or missile. The two wounds must have been caused by the same agent (earlier known as double perfora ti on). c) lntraocular foreign body injury is technically a penetra ti ng injury associated with retained intraocular foreign body. However, it is grouped separately because of di ff erent clinical implica ti ons.
- 5. PENETRATING INJURY PERFORATING INJURY OPEN GLOBE INJURY
- 6. Extraocular foreign bodies are quite common in industrial and agricultural workers. Even in day-to day life, these are common. Common sites and types Common sites A foreign body may be impacted in the conjunc ti va or cornea • On the conjunc ti va, it may be lodged in the sulcus subtarsalis, fornices or bulbar conjunc ti va. • In the cornea, it is usually embedded in the epithelium, or super fi cial stroma and rarely into the deep stroma. Common types common foreign bodies are par ti cles of dust, sand, steel, glass, wood and small insects. Clinical features Symptoms • Discomfort, profuse watering and redness in the eye. • Pain and photophobia are more marked in corneal foreign body than the conjunc ti va. • Defec ti ve vision occurs when it is lodged in the centre of cornea. Signs • Blepharospasm and conjunc ti val conges ti on. • A foreign body can be localized on the conjunc ti va or cornea by oblique illumina ti on. • Slit-lamp examina ti on a ft er fl uorescein staining is the best method to discover corneal foreign body. • Double eversion of the upper lid is required to discover a foreign body in the superior fornix. EXTRAOCULAR INJURIES
- 7. Complica ti ons 1. Acute bacterial conjunc ti vi ti s 2. Corneal ulcera ti on 3. Pigmenta ti on and/or opacity may be le ft behind Treatment Extraocular foreign bodies should be removed as early as possible. 1.Removal of conjunc ti val foreign body A foreign body lying loose in the lower fornix, sulcus subtarsalis or in the canthi may be removed with a swab s ti ck or clean handkerchief even without anaesthesia. Foreign bodies impacted in the bulbar conjunc ti va need to be removed with the help of a hypodermic needle a ft er topical anaesthesia. 2.Removal of corneal foreign body. I. Eye is anaesthe ti sed with topical ins ti lla ti on of 2 to 4% xylocaine and the pa ti ent is made to lie supine on an examina ti on table. II. Lids are separated with universal eye speculum, the pa ti ent is asked to look straight upward and light is focused on the cornea. III. First of all, an a tt empt is made to remove the foreign body with the help of a wet co tt on swap s ti ck. If it fails then foreign body spud or hypodermic needle is used. IV. Extra care is taken while removing a deep corneal foreign body, as it may enter the anterior chamber during manoeuvring. V. If such a foreign body happens to be magne ti c, it is removed with a hand-held magnet.
- 8. XYLOCAINE 4% HAND-HELD MAGNET VI. A ft er removal of foreign body, patching with an ti bio ti c eye ointment is applied for 24 to 48 hours. VII. An ti bio ti c eyedrops are ins ti lled 3-4 ti mes a day for about a week. UNIVERSAL EYE SPECULUM
- 9. BLUNT TRAUMA CAUSES AND PATHOGENESIS OF DAMAGE Modes of trauma • Direct blow to the eyeball by fi st, a tennis or cricket or another ball or blunt instruments like s ti cks, and big stones. • Accidental blunt trauma to eyeball may also occur in roadside accidents, automobile accidents, injuries by agricultural and industrial instruments/machines and fall upon the projec ti ng bluntobjects Mechanics of forces of blunt trauma Blunt trauma of eyeball produces damage by di ff erent forces as described below: 1. Direct impact on the globe. It produces maximum damage at the point where the blow is received. 2. Compression wave force. It is transmi tt ed through the fl uid contents in all the direc ti ons and strikes the angle of anterior chamber, pushes the iris-lens posteriorly, and also strikes the re ti na and Choroid. Some ti mes, the compression wave may be so explosive, that maximum damage may be produced at a point distant from the actual place of impact. This is called contre- coup damage. 3. Re fl ected compression wave force. A ft er striking the outer coats, the compression waves are re fl ected towards the posterior pole and may cause foveal damage.
- 10. DIRECT IMPACT COMPRESSION WAVE FORCE REFLECTED COMPRESSION WAVE MECHANICS OF BLUNT TRAUMA TO EYEBALL
- 11. 4. Rebound compression wave force. A ft er striking the posterior wall of the globe, the compression waves rebound back anteriorly. This force damages the re ti na and choroid by forward pull and lens iris diaphragm by forward thrust from the back. 5. Indirect force. Ocular damage may also be caused by the indirect forces from the bony walls and elas ti c contents of the orbit, when globe suddenly strikes against these structures. REBOUND COMPRESSION WAVE FORCE
- 12. TRAUMATIC LESIONS OF BLUNT TRAUMA Trauma ti c lesions produced by blunt trauma can be grouped as follows: A. Closed-globe injury B. Globe rupture C. Extraocular lesions A. Closed-globe injury Either there is no corneal or scleral wound at all (contusion) or it is only of par ti al thickness (lamellar lacera ti on). Contusional injuries may vary in severity from a simple corneal abrasion to an extensive intraocular damage. I. Cornea 1. Simple abrasions. These are very painful and diagnosed by fl uorescein staining. These usually heal up within 24 hours with patching applied a ft er ins ti lling an ti bio ti c ointment. 2. Par ti al corneal tears (lamellar corneal lacera ti on). These may also follow a blunt trauma and are treated by topical an ti bio ti cs and patching. 3. Acute corneal oedema may occur following trauma ti c dysfunc ti on of endothelial cells. It may be associated with Descemet’s folds and stromal thickening. It, usually, clears up spontaneously; rarely a deep corneal opacity may be the sequelae.
- 13. 4. Blood staining of cornea. It may occur occasionally from the associated hyphaema and raised intraocular pressure. Cornea becomes reddish brown or greenish in colour and in later stages simulates disloca ti on of the clear lens into the anterior chamber. It clears very slowly from the periphery towards the centre, the whole process may take even more than two years. BLOOD STAINING OF CORNEA
- 14. II. Sclera Par ti al thickness scleral wounds (lamellar scleral lacera ti ons) may occur alone or in associa ti on with other lesions of closed-globe injury. III. Anterior chamber 1. Trauma ti c hyphaema (blood in the anterior chamber). It occurs due to injury to the iris or ciliary body vessels. HYPHAEMA
- 15. ■ Treatment includes: • Conserva ti ve treatment is aimed at preven ti on of rise in IOP and occurrence of secondary haemorrhage (re-bleed). • Surgical treatment. A small hyphaema usually clears up with conserva ti ve treatment. A large non resolving hyphaema causing raised IOP should be drained to avoid blood staining of the cornea. 2. Exudates. These may collect in the anterior chamber following trauma ti c uvei ti s. IV. Iris, pupil and ciliary body 1. Traumatic miosis. It occurs ini ti ally due to irrita ti on of ciliary nerves. It may be associated with spasm of accommoda ti on. 2. Traumatic mydriasis (Iridoplegia). It is usually permanent and may be associated with trauma ti c cycloplegia. 3. Rupture of the pupillary margin is a common occurrence in closed-globe injury.
- 16. RUPTURE OF PUPILLARY MARGIN
- 17. 4. Iridodialysis, i.e., detachment of iris from its root at the ciliary body occurs frequently. It results in a D-shaped pupil and a black biconvex area seen at the periphery. 5. An ti fl exion of the iris. It refers to rota ti on of the detached por ti on of iris, in which its posterior surface faces anteriorly. It occurs following extensive iridodialysis. 6. Retro fl exion of the iris. This term is used when whole of the iris is doubled back into the ciliary region and becomes invisible. 7. Trauma ti c aniridia or iridemia. In this condi ti on, the completely torn iris (from ciliary body) sinks to the bo tt om of anterior chamber in the form of a minute ball. 8. Angle recession refers to the tear between longitudinal and circular muscle fi bres of the ciliary body. It is characterized by deepening of the anterior chamber and widening of the ciliary body band on gonioscopy. Later on, it is complicated by glaucoma. 9. In fl ammatory changes. These include trauma ti c iridocycli ti s, haemophthalmi ti s, post-trauma ti c iris atrophy and pigmentary changes. Treatment. It consists of atropine, an ti bio ti cs and steroids. In the presence of ruptures of pupillary margins and subluxa ti on of lens, atropine is contraindicated.
- 19. V. Lens 1. Vossius ring. It is a circular ring of brown pigment seen on the anterior capsule. It occurs due to striking of the contracted pupillary margin against the crystalline lens. It is always smaller than the size of the pupil. VOSSIOUS RING
- 20. 2. Concussion cataract. It occurs mainly due to imbibi ti on of aqueous and partly due to direct mechanical e ff ects of the injury on lens fi bres. • Discrete subepithelial opaci ti es are of most common occurrence. • Early rose tt e cataract (punctate). It is the most typical form of concussion cataract. It appears as feathery lines of opaci ti es along the star-shaped suture lines; usually in the posterior cortex. • Late rose tt e cataract. It develops in the posterior cortex 1 to 2 years a ft er the injury. Its sutural extensions are shorter and more compact than the early rose tt e cataract. • Di ff use (total) concussion cataract. It is of frequent occurrence. ROSETTE CATARACT
- 21. 3. Trauma ti c absorp ti on of the lens. It may occur some ti mes in young children resul ti ng in aphakia. 4. Subluxa ti on of the lens. It may occur due to par ti al tear of zonules. The subluxated lens is slightly displaced but s ti ll present in the pupillary area. Subluxated lens may cause trembling of the iris (iridodonesis) and/or trembling of lens (phacodonesis). 5. Disloca ti on of the lens. It occurs when rupture of the zonules is complete. It may be intraocular or extraocular. Intraocular disloca ti on may be anterior or posterior. Extraocular disloca ti on may be in the subconjunc ti val space. SUBLUXATION ANTERIOR DISLOCATION POSTERIOR DISLOCATION DISPLACEMENTS OF LENS
- 22. VI. Vitreous 1. Liquefac ti on and appearance of clouds of fi ne pigmentary opaci ti es (a most common change). 2. Detachment of the vitreous either anteriorly at the base or posterior (PVD) may occur. 3. Vitreous haemorrhage. It is of common occurrence 4. Vitreous hernia ti on in the anterior chamber may occur with subluxa ti on or disloca ti on of the lens. VITREOUS HAEMORRHAGE
- 23. VII. Choroid 1. Rupture of the choroid. The rupture of choroid is concentric to the op ti c disc. Rupture may be single or mul ti ple. On fundus examina ti on, the choroidal rupture looks like a whi ti sh crescent (due to underlying sclera) with fi ne pigmenta ti on at its margins. Re ti nal vessels pass over it. CHOROIDAL RUPTURE
- 24. 2. Choroidal haemorrhage may occur under the re ti na (subre ti nal) or may even enter the vitreous if re ti na is also torn. 3. Choroidal detachment is also known to occur following blunt trauma. CHOROIDAL HAEMRRHAGE CHOROIDAL DETACHMENT
- 25. VIII. Re ti na 1. Commo ti o re ti nae. It is of common occurrence following a blow on the eye. It manifests as a considerable area of the posterior pole with a ‘cherry-red spot’ in the foveal region. It may disappear a ft er some days or may be followed by pigmentary changes COMMOTIO RETINAE
- 26. 2. Re ti nal haemorrhages. These are quite common following concussion trauma. Mul ti ple haemorrhages including fl ame-shaped. 3. Re ti nal tears. 4. Re ti nal detachment. 5. Concussion changes at macula. Trauma ti c macular oedema is usually followed by pigmentary degenera ti on. Some ti mes, a macular cyst is formed, which on rupture may be converted into a lamellar or full thickness macular hole. RETINAL HAEMORRHAGE
- 27. B. Globe rupture Globe rupture is a full-thickness wound of the eyeball (sclera, cornea or both) caused by a blunt object. Types of globe rupture Globe rupture may occur in two ways: 1. Direct rupture may occur, though rarely, at the site of injury. 2. Indirect rupture is more common and occurs because of the compression force. The impact results in momentary increase in the intraocular pressure and an inside-out injury at the weakest part of eyewall. Clinical features Rupture of the globe may be associated with: Prolapse of uveal ti ssue, vitreous loss, intraocular haemorrhage and disloca ti on of the lens. • Intraocular pressure may be raised ini ti ally, but ul ti mately it is decreased. • Accompanying signs include irregular pupil, hyphaema, commo ti o re ti nae, choroidal rupture, and re ti nal tears. Treatment • Repair of tear in the eyewall should be done under general anaesthesia to save the eyeball whenever possible. • Postopera ti ve treatment should include an ti bio ti cs, steroids and atropine. • Enuclea ti on may be required in a badly damaged eye where salva ti on is not possible.
- 28. C. Extraocular lesions 1. Conjunctival lesions include: • Subconjunctival haemorrhage occurs very commonly. It appears as a bright red spot. • Chemosis and lacerating wounds of conjunctiva (tears) are also not uncommon SUBCONJUNCTIVAL HAEMORRAGE
- 29. 2. Eyelid lesion include: • Ecchymosis of eyelids is of frequent occurrence. • Lacera ti on and avulsion of the lids. • Trauma ti c ptosis may follow damage to the levator muscle. 3. Lacrimal apparatus lesions 4. Op ti c nerve injuries 5. Orbital injury ECCHYMOSIS OF EYELID LACERATION AND AVULSION
- 30. OPEN-GLOBE INJURIES Modes of injury 1. Trauma by sharp and pointed instruments like needles, knives, nails, arrows, screw-drivers, pens, pencils, compasses, glass pieces and so on. 2. Trauma by foreign bodies travelling at very high speed such as bullet injuries and iron foreign bodies in lathe workers. Mechanisms of damage 1. Mechanical effects of the trauma or physical changes. 2. Introduction of infection. 3. Post-traumatic iridocyclitis. It is of frequent occurrence and if not treated properly can cause devastating damage, a rare but most dangerous complication of a perforating injury Trauma ti c lesions with management 1. Wounds of the conjunc ti va. These are common and usually associated with subconjunc ti val haemorrhage. A wound of more than 3 mm should be sutured. 2. Wounds of the cornea. These can be divided into uncomplicated and complicated wounds. i.Uncomplicated corneal wounds. These are not associated with prolapse of intraocular contents. Treatment. A small central wound does not need s ti tching. The only treatment required is pad and bandage with atropine and an ti bio ti c ointments. A large corneal wound (more than 2 mm) should always be sutured.
- 31. ii.Complicated corneal wounds. These are associated with prolapse of iris, some ti mes lens ma tt er and even vitreous. Treatment. Corneal wounds with iris prolapse should be sutured a ft er abscising the iris. The prolapsed iris should never be reposited; since it may cause infec ti on. When associated with lens injury and vitreous loss, lensectomy and anterior vitrectomy may be performed along with repair of the corneal wound. CORNEAL TEAR WITH IRIS PROLAPSE
- 32. 3. Wounds of the sclera. These are usually associated with corneal wounds and should be managed as above. In corneo-scleral tear, fi rst suture should be applied at the limbus. 4. Wounds of the lens. Extensive lens ruptures with vitreous loss should be managed as above. Small wounds in the anterior capsule may seal and lead on to trauma ti c cataract. 5. A badly (severely) wounded eye. It refers to extensive corneo-scleral tears associated with prolapse of the uveal ti ssue, lens rupture, vitreous loss and injury to the re ti na and choroid. Usually there seems to be no chance of ge tti ng useful vision in such cases. So, preferably such eyes should be excised. INTRAOCULAR FOREIGN BODIES Penetra ti ng injuries with foreign bodies are not infrequent. Seriousness of such injuries is compounded by the reten ti on of intraocular foreign bodies (IOFB). Common foreign bodies chips of iron and steel (90%), par ti cles of glass, stone, lead pellets, copper percussion caps, aluminium, plas ti c and wood. Modes of damage and lesions A penetra ti ng/perfora ti ng injury with retained foreign body may damage the ocular structures by the following modes:
- 33. A. Mechanical e ff ects. B. Introduc ti on of infec ti on. C. Reac ti on of foreign bodies. D. Post-trauma ti c iridocycli ti s. A. Mechanical e ff ects Mechanical e ff ects depend upon the size, velocity and type of the foreign body. Foreign bodies greater than 2 mm in size cause extensive damage. The lesions caused also depend upon the route of entry and the site up to which a foreign body has travelled. Trauma ti c lesions produced by intraocular foreign bodies include: • Corneal or/and scleral perfora ti on, hyphaema, iris hole, • Rupture of the lens and trauma ti c cataract, • Vitreous haemorrhage and/or degenera ti on, • Choroidal perfora ti on, haemorrhage and in fl amma ti on, • Re ti nal hole, haemorrhages, oedema and detachment. Loca ti ons of IOFB. Having entered the eye through the cornea or sclera a foreign body may be retained at any of the following sites 1. Anterior chamber. In the anterior chamber, the IOFB usually sinks at the bo tt om. A ti ny foreign body may be concealed in the angle of anterior chamber, and visualised only on gonioscopy. 2. Iris. Here the foreign body is usually entangled in the stroma.
- 34. 3. Posterior chamber. Rarely, a foreign body may sink behind the iris a ft er entering through pupil or a ft er making a hole in the iris. 4. Lens. Foreign body may be present on the anterior surface or inside the lens. Either an opaque track may be seen in the lens or the lens may become completely cataractous. 5. Vitreous cavity. A foreign body may reach here through various routes. 6. Re ti na, choroid and sclera. A foreign body may obtain access to these structures through corneal route or directly from scleral perfora ti on. 7. Orbital cavity. A foreign body piercing the eyeballmay occasionally cause double perfora ti on and come to rest in the orbital ti ssues. Management of retained intraocular foreign bodies (IOFB) Diagnosis. It is a ma tt er of extreme importance par ti cularly as the pa ti ent is o ft en unaware that a par ti cle has entered the eye. To come to a correct diagnosis following steps should be taken: 1.History 2.Ocular examina ti on 3.Plain X-rays 4.B scan 5.CT 6.MRI
- 35. 1, ANTERIOR CHAMBER; 2, IRIS; 3, LENS; 4, VITREOUS; 5, RETINA; 6, CHOROID; 7, SCLERA; 8, ORBITAL CAVITY COMMON SITES FOR RETENTION OF AN INTRAOCULAR FOREIGN BODY DEPICTION OF ROUTES OF ACCESS OF A FOREIGN BODY IN THE VITREOUS
- 36. TREATMENT IOFB should always be removed, except when it is inert and probably sterile or when li tt le damage has been done to the vision and the process of removal may be risky and destroy sight (e.g., minute FB in the re ti na). 1. Foreign body in the anterior chamber. It is removed through a corresponding corneal incision directed straight towards the foreign body. 2. Foreign body entangled in the iris ti ssue (magne ti c as well as non-magne ti c) is removed by performing sector iridectomy of the part containing foreign body. 3. Foreign body in the lens.Magnet extrac ti on is usually di ffi cult for intralen ti cular foreign bodies. Therefore, magne ti c foreign body should also be treated as non magne ti c foreign body. An extracapsular cataract extrac ti on (ECCE) with intraocular lens implanta ti on should be performed. The foreign body may be evacuated itself along with the lens ma tt er or may be removed with the help of forceps. 4.Foreign body in the vitreous and the re ti na is removed as follow: i.Magne ti c removal. This technique is used to remove a magne ti c foreign body that can be well localized and removed safely with a powerful magnet without causing much damage to the intraocular structures.
- 37. ii.Forceps removal with pars plana vitrectomy. This technique is used to remove all non-magne ti c foreign bodies and those magne ti c foreign bodies that cannot be safely removed with a magnet. In this technique, the foreign body is removed with vitreous forceps a ft er performing three-pore pars plana vitrectomy under direct visualiza ti on using an opera ti ng microscope. REMOVAL OF A MAGNETIC INTRAOCULAR FOREIGN BODY FROM POSTERIOR SEGMENT REMOVAL OF A NON-MAGNETIC FOREIGN BODY THROUGH PARS PLANA
- 38. CHEMICAL INJURIES Chemical injuries are by no means uncommon. These vary in severity from a transient irrita ti on of li tt le signi fi cance to complete and sudden loss of vision. Modes of chemical injury These usually occur due to external contact with chemicals under following circumstances: 1. Domes ti c accidents, e.g., with ammonia, solvents, detergents and cosme ti cs. 2. Agricultural accidents, e.g., due to fer ti lizers, insec ti cides, toxins of vegetable and animal origin. 3. Chemical laboratory accidents, with acids and alkalies. 4. Deliberate chemical a tt acks, especially with acids to dis fi gure the face. 5. Self-in fl icted chemical injuries are seen in psychopaths. Types of chemical injuries In general, the serious chemical burns mainly comprise alkali and acid burns. A. Alkali burns • Alkali burns are among the most severe chemical injuries known to the ophthalmologists. • Common alkalies responsible for burns are: lime, caus ti c potash or caus ti c soda and liquid ammonia (most harmful).
- 39. Mechanisms of damage produced by alkalies includes: 1. Alkalies dissociate and saponify fa tt y acids of the cell membrane and, therefore, destroy the structure of cell membrane of the ti ssues. 2. Being hygroscopic, they extract water from the cells, a factor which contributes to the total necrosis. 3. They combine with lipids of cells to form soluble compounds, which produce a condi ti on of so ft ening and gela ti nisa ti on B. Acid burns • Acid burns are less serious than alkali burns. • Common acids responsible for burns are: sulphuric acid, hydrochloric acid and nitric acid. Chemical e ff ects. Strong acids cause instant coagula ti on of all the proteins which then act as a barrier and prevent deeper penetra ti on of the acids into the ti ssues. Thus, the lesions become sharply demarcated. Treatment of chemical burns 1. Prevent further damage Immediate and thorough irriga ti on with the available clean water or saline delivered through an IV tubing. Deliver minimum of 2 L of water in 20-30 minutes or un ti l pH is restored. Mechanical removal of contaminant. • If any par ti cles are le ft behind, par ti cularly in the case of lime, these should be removed carefully with a swab s ti ck. • Removal of contaminated and necro ti c ti ssue. • Necrosed conjunc ti va should be excised. • Contaminated and necrosed corneal epithelium should be removed with a co tt on swab s ti ck.
- 40. A PATIENT WITH CHEMICAL INJURY FACE INCLUDING EYE 2. Maintenance of favourable condi ti onsfor rapid and uncomplicated healing by following measures: • Topical an ti bio ti c dropse.g., moxi fl oxacin 4-6 ti mes a day to prevent infec ti on. • Steroid eye drops • Cycloplegics, e.g., atropine, may improve the comfort. • Ascorbic acid, in the form of 10% sodium ascorbate eyedrops (4-5 ti mes) • Lubricant eyedrops (preserva ti ve free) should be used in abundance to promote the healing. • Sodium citrate, used as 10% topical eyedrops stabilizes neutrophils and reduces collagenase release.
- 41. 3. Preven ti on of symblepharon can be done by using a glass shell or sweeping a glass rod in the fornices twice daily. 4. Treatment of complica ti ons, as below: • Secondary glaucoma should be treated by topical 0.5% ti molol, ins ti lled twice a day along with oral acetazolamide 250 mg 3-4 ti mes a day. • Pseudopterygium, when formed, should be excised together with conjunc ti val autogra ft • Symblepharon needs surgical treatment. • Corneal opacity may be treated by keratoplasty if adequate tear fi lm and stem cell popula ti on available. • Keratoprosthesis remains a surgical op ti on in severely damaged eyes where keratoplasty is not possible. PTERYGIUM PSEUDOPTERYGIUM
- 42. THANKS